Ketamine for PTSD
PTSD continues to be a problematic psychiatric condition that can be difficult to treat. SSRIs are the first-line treatment, and they are the only pharmaceutical class approved – their use may lead to a reduction in symptoms, but often, PTSD can be found to be treatment resistant. This is where Ketamine PTSD therapy can be an option.
Atypical antipsychotics such as quetiapine and risperidone are sometimes used clinically to control these symptoms. Benzodiazepines are used at times, but with caution, as individuals suffering from PTSD are at heightened risk for addiction.
Given this, novel treatments are needed for complex PTSD symptoms. One such treatment could be ketamine. As noted, there is some hesitation for its use because it may cause transient dissociation; however, more recent studies suggest that this may not be as frequent as previously thought.
With more ketamine and PTSD investigation, ketamine may be a viable tool for treating PTSD for those who fail more conventional treatments.
Ketamine is a controversial controlled medication gaining popularity in its off-label use in treatment-resistant MDD. It is noted to have an ultra-rapid onset of efficacy but also is limited by its offset of effect over 1–2 weeks. [1]
What is Ketamine?
Ketamine is a structural analog of the dissociative anesthetic and recreational drug phencyclidine (PCP). Originally called CI-581, ketamine has one-tenth the potency of PCP and causes less severe dysphoria and hallucinations. [2]
Intramuscular and intravenous ketamine is commonly used to provide pediatric anesthesia, especially for high-risk children or patients in limited-resource settings. In surgical settings, ketamine is typically combined with benzodiazepines, reducing the adverse psychological symptoms that occur during emergence. Off-label, subanesthetic doses of ketamine are also used for acute and chronic pain management, sedation, and severe depression treatment.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Dual Diagnosis Mental Health Centers Near You?
Even if therapy failed previously, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about counseling alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
FREE 24/7 Dual Diagnosis Mental Health Services HotlineKetamine Therapy for PTSD
Post-traumatic stress disorder (PTSD) is the presence of recurrent, intrusive distressing memories, dreams, dissociative reactions such as flashbacks, and reactions to internal or external cues that symbolize or resemble an aspect of a traumatic event experienced by an individual. The traumatic event can be an actual or threatened case of death, serious injury, or sexual assault that affected an individual, close friend, or family member.
In response to these symptoms, individuals often attempt to avoid situations where they may be reminded about the trauma internally by controlling thoughts, memories, and emotions or externally by avoiding people, places, conversations, and situations that can trigger memories regarding the traumatic event. They may also exhibit changes in memory formation. For example, they may display selective amnesia – the inability to remember specific details surrounding the trauma unrelated to external causes such as substance use and physical trauma.
They may also develop a constellation of symptoms that mirrors major depressive disorder (MDD), including negative beliefs and expectations, negative emotional states, anhedonia, and social withdrawal. In addition to these symptoms, patients may experience changes in emotional reactivity, including irritability, self-destructive behavior, hypervigilance, sleep disturbance, and lack of concentration.
PTSD’s prevalence is 8.7% in the United States, with a prevalence of 3.5% during any given 12-month period. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), PTSD is more prevalent among military veterans, firefighters, police officers, and emergency medical personnel. Globally, the greatest prevalence is found among survivors of rape, military combat and captivity, and politically motivated genocide. [3]

The Veteran’s Administration/Department of Defense currently includes the use of selective serotonin reuptake inhibitors (SSRIs) for use as pharmacotherapy for PTSD. The SSRIs included in this recommendation are sertraline and paroxetine. Although SSRIs are one of the primary modes of pharmacotherapy for PTSD, many drugs may also be used. For example, serotonin-norepinephrine reuptake inhibitors (SNRIs), such as venlafaxine, are also listed as a recommendation for monotherapy in PTSD. Other drugs that may be used include imipramine and phenelzine – a tricyclic antidepressant (TCA) and monoamine oxidase inhibitor. However, these medications are listed cautiously, as they may have potentially serious side effects. One novel treatment not typically included in guidelines is ketamine PTSD veterans treatment.
Some researchers suggest that a loss of synaptic connectivity may cause the symptoms experienced in complex trauma and PTSD. The stress experienced in PTSD may impair the functioning of synaptic connectivity, which is mostly mediated by glutamate. As glutamate synapses play a crucial role in these neuronal circuits, using ketamine treatment for PTSD may enhance synaptic connectivity in these circuits, ultimately reversing the effects of stress. Other researchers have examined how prophylactic use of ketamine may have a protective effect against the development of stress-related disorders. [4]

End the Emotional Pain. Get Your Life Back.
Feeling Depressed, Anxious or Struggling with Mental Health Illness? Get Safe Comfortable Mental Health Dual Diagnosis High-Quality Therapy From Counselors That Care. Begin Your Recovery Now.
Hotline (855) 940-6125How Does Ketamine Help PTSD?
Ketamine drug has been traditionally used as an alternative to general anesthesia. It produces ‘dissociation’ between the thalamaco-neocortical and limbic systems. This dissociation is thought to be both functional and electrophysiological. Clinically, individuals given ketamine exhibit a state of catalepsy in which the eyes remain open and have slow nystagmus. During this state, the individuals maintain corneal and light reflexes.6 Patients become flaccid but are awake. [5]
Ketamine activity occurs as an antagonist at the N-methyl-D-aspartate-type glutamate (NMDA) receptor. It has been studied in greater detail recently due to its potential use as an antidepressant agent.10 NMDA receptor activation has been shown to increase the formation of spontaneous intrusive memories (depressive or anxious), and high activity of the NMDA receptor may be a risk factor for actually developing PTSD. As ketamine functions as an antagonist to the NMDA receptor, it may be a promising drug target to lower PTSD symptoms as such.
First-class Facilities & Amenities
World-class High-Quality Mental Health Services & Behavioral Health Substance Abuse Treatment
Rehab Centers TourRenowned Mental Health Centers. Serene Private Facilities. Inpatient Rehab Programs Vary.
Mental Health Helpline (855) 940-6125Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Successes
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Development Events
- Comfortable Onsite Medical Detox Center
How Ketamine Works?
Ketamine is an N-methyl-d-Aspartate receptor agonist with well-established safety and efficacy as an analgesic and anesthetic. Since ketamine was developed in 1964, largely as a replacement for phencyclidine, it has been used primarily in veterinary and pediatric anesthesia. Still, interest in recent years has burgeoned in psychiatry after reports of its rapid-acting antidepressant effects. The potential for ketamine to be used in treating psychiatric disorders was first noted in the 1970s and has been the focus of the formal investigation since the 1990s, with investigative and off-label use in the context of mental health increasing across North America and Europe since that time.
The first approval by the USA Food and Drug Administration (FDA) of a ketamine-derived therapy for mental health came in 2019 for intranasal esketamine (the S-enantiomer of ketamine) as augmentation therapy for treatment-resistant depression, which has increased clinical and public interest internationally. [7]

World-class, Accredited, 5-Star Reviewed, Effective Mental Health Dual Diagnosis Programs. Complete Integrated Inpatient Rehab with Free Post Discharge Therapy Planning.
CALL (855) 940-6125End the Emotional Pain Rollercoaster. Gain Stability & Happiness Through Recovery Treatment. Start Mental Health Counseling Today. Get Free No-obligation Guidance by Behaviroal Health Specialists Who Understand Mental Health Recovery.
Ketamine Infusion PTSD
Conventional therapies for PTSD include cognitive and family therapy and medications. These treatments take time to work, and sometimes, men and women with PTSD get little relief from their condition. If your PTSD is resistant to these treatments, PTSD ketamine therapy may be an option.
Ketamine, used primarily in anesthesia, has notable effects on the symptoms of PTSD when administered in lower doses than those used for anesthesia. Research shows that even a single infusion can decrease depressed mood and anxiety in patients with severe depression — including those with PTSD.
Ketamine for PTSD and Depression
Major depressive illness is a debilitating condition that is a matter of concern worldwide, affecting millions of people and causing a considerable burden on health and socioeconomic status. [6] As per the World Health Organization, depression is third among the global disease burden.
Recently, ketamine has been used more widely due to its approval for treatment-resistant depression (TRD). TRD is a severe depression that has not improved via other therapies, including people experiencing suicidal thoughts.
The administration of slow i.v ketamine in patients with severe depression results in significant improvement in depression and anxiety symptoms immediately 1 h after a single dose. This effect is sustained with repeated six doses over 2 weeks. There is an overall decrease in illness severity after 2 weeks. This provides substantiative evidence for ketamine’s rapid and sustained effective role in depressive disorders and its tolerability at a subanesthetic dose of 0.5 mg/kg body weight by i.v bolus injection. Ketamine infusion cost for depression is about $400 to $2000 for each session, depending on the location, the clinic, and your condition.
Ketamine for PTSD and Anxiety
Results from the clinical trials on ketamine therapy show that at-home ketamine therapy is a secure and efficient technique to treat anxiety and depressive symptoms. While ketamine for PTSD treatment may relieve some patients from anxiety or depression, doctors warn that additional study is still required to fully understand how it differs from more conventional therapies.
Physicians may prescribe ketamine, but they will still be subject to their state’s laws on licensure.
Ketamine for PTSD Side Effects
The most common adverse effects associated with ketamine administration were increases in systolic and diastolic blood pressure, dissociation, and psychotomimetic symptoms, all of which were short-lived. However, given the relatively nascent state of research and practice in ketamine for mental health, further research is required to determine the safety and tolerability of ketamine in psychiatric populations, particularly over the longer term. Nonetheless, extant evidence on the risks of ketamine suggests a profile that is comparable to other widely used psychiatric medications.
Ketamine overdose symptoms are similar to PCP overdose, although the effects of ketamine tend to resolve more quickly. Physical signs and symptoms are dose-dependent through the loss of consciousness. Patients may be unable to provide a relevant history, and clinicians should seek pertinent clinical information from witnesses. Clinicians should also maintain familiarity with street names for ketamine.
The following symptoms may be present during ketamine use and intoxication:
- General – sedation, impaired consciousness
- Head, Ear, Eyes, Nose, Throat – horizontal, vertical or rotary nystagmus, mydriasis, excessive salivation
- Cardiovascular – hypertension, tachycardia, palpitations, arrhythmias, chest pain
- Abdominal – abdominal pain, abdominal tenderness, nausea, vomiting
- Neurological – altered mental status (disorientation), paranoia, dysphoria, anxiety, confusion, slurred speech, dizziness, ataxia, dysarthria, trismus, muscular rigidity, psychomotor, psychomimetic, or acute dystonic reactions
- Genitourinary – lower urinary tract symptoms
- Trauma – a thorough examination for evidence of trauma is needed as injuries secondary to ketamine intoxication can occur due to the diminished perception of pain.
Symptoms mostly unique to overdose, overly rapid infusion, or combined with other drugs include:
- Respiratory – respiratory depression, apnea
- Cardiovascular – hypotension, bradycardia, myocardial infarction
- Neurological – seizure, stupor, coma
Symptoms mostly unique to iatrogenic, intravenous delivery include:
- Respiratory – respiratory depression, laryngospasm
Ketamine Addiction Signs
The following are signs that you, or someone you know, may be struggling with ketamine addiction.
Psychological ketamines addictive symptoms:
- Euphoria
- Distorted perception of reality, space, and time
- Floating/flying sensation
- Entering into a trance-like state
- Feeling detached from your body and surroundings, leading to an out-of-body experience or causing you to believe that you have died
- Depression
- Anxiety
- Fear, paranoia, and intense confusion
- Memory problems
- Auditory or visual hallucinations (hearing or seeing things that aren’t truly there)
- Inability to focus or concentrate
- Consuming ketamine to try and relieve stress; can often be the trigger for many people who go on to become addicted to ket
- Exacerbation of any existing mental health challenges

Behavioral and social symptoms of ketamine addiction:
- Using ketamine regularly in your day-to-day life and feeling as though you are unable to function without it
- Devoting an excessive amount of time to obtaining, using, and recovering from the effects of ketamine consumption
- Feeling as though you want to stop taking ketamine but finding that you are unable to
- Inability to stop thinking about when, where, and how you will get your next fix of ketamine
- Feeling as though ketamine has taken over your life
- Taking ketamine has become more important than hobbies or activities that you once enjoyed
- Continuing to take ketamine, even after experiencing negative consequences as a result of your ketamine abuse
- Mixing ketamine with other addictive drugs or alcohol
- Seeking out new ways to consume ketamine to experience a more intense high
- Being defensive, dishonest, and secretive about your ketamine use
- Withdrawing from loved ones leads to social isolation
- Finding that you only tend to socialize with people who take ketamine or other drugs
- People have noticed dramatic changes in your appearance or behavior as a result of your ketamine use
- Neglecting your responsibilities due to being high on ket
- Poor performance and attendance at work
- Stealing money or selling valuables to pay for ketamine
- Possession of paraphernalia related to injecting ketamine e.g. needles, syringes
- Engaging in risky and reckless behaviors when under the influence of ketamine
Physical ketamine addiction symptoms:
- Gradually building a tolerance to ketamine, meaning that you need to take higher doses of this drug and more frequently to experience the desired high
- Experiencing withdrawal symptoms if you stop taking or significantly reduce your ketamine use
- Scabs and bruises on the skin as a result of injecting ketamine
- Tiredness and fatigue
- Inability to feel pain
- Increased heart rate
- Breathing problems
- Co-ordination problems
Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.
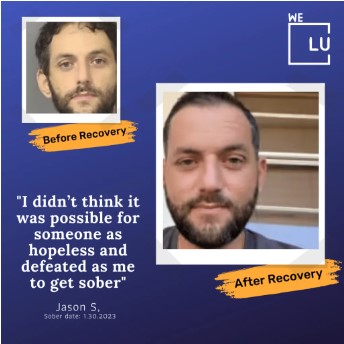


Start a New Life
Begin with a free call to a behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- Comfortable Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
PTSD Treatment
Posttraumatic stress disorder (PTSD) is a chronic, often debilitating mental health disorder that may develop after a traumatic life event, such as military combat, natural disaster, sexual assault, or unexpected loss of a loved one. Most of the U.S. population is exposed to a traumatic event during their lifetime, and shortly after exposure, many people experience some symptoms of PTSD. Although among most individuals, these symptoms resolve within several weeks, approximately 10%-20% of individuals exposed to trauma experience PTSD symptoms that persist and are associated with impairment. [4]
The diagnosis of what is now accepted as Post Traumatic Stress Disorder (PTSD) has changed over the years as we have gained a better understanding of the stress response and its longer-term impact on the body and the brain. PTSD treatment works. Those who have gone through trauma can learn to feel safe in the world and cope with stress.
Deciding to get help and taking steps to start can be hard. There are several effective PTSD treatments. This means you have options. Many professionals provide evidence-based talk therapy and medication to people who go through trauma. Treatments with the strongest evidence should be the first line of treatment for PTSD whenever possible, considering patient preferences, values, and clinician expertise.
Searching for “ketamine for PTSD near me?” With more investigation, ketamine PTSD therapy may prove to be a viable tool in PTSD treatment for those who fail more conventional treatments.
We Level Up FL provides world-class care with round-the-clock medical professionals available to help you cope. All work as a team, providing mental health treatment for successful recovery. Make this your opportunity to reclaim your life. Call today to speak with one of our treatment specialists. Your call is private and confidential, and there is never any obligation.
Search Ketamine PTSD & Other Resources
Sources:
[1,3,4] Liriano F, Hatten C, Schwartz TL. Ketamine as a treatment for post-traumatic stress disorder: a review. Ketamine PTSD Drugs Context. 2019 Apr 8;8:212305. DOI: 10.7573/dic.212305. PMID: 31007698; PMCID: PMC6457782. – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6457782/
[2] Orhurhu VJ, Vashisht R, Claus LE, et al. Ketamine Toxicity. [Updated 2022 Apr 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541087/
[5] White PF, Way W, Trevor AJ. Ketamine—its pharmacology and therapeutic uses. Anesthesiology. 1982;56(2):119–136. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6457782/
[6] NCBI – The correlation between ketamine and posttraumatic stress disorder in burned service members. J Trauma. 2008;64:S195–S199. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6457782/
[7] NCBI – Ketamine for treating mental health and substance use disorders: a comprehensive systematic review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8715255/