What are the Most Effective Medications for Postpartum Depression?
Postpartum depression is a mood disorder that can occur after childbirth. It may affect self-care and the ability to care for the baby, often requiring support and, in some cases, medical intervention. Your doctor might recommend antidepressants for postpartum depression symptoms. Antidepressants are effective in helping regulate mood-affecting brain chemicals. If you’re breastfeeding, discuss the risks and benefits with your doctor, as some antidepressants can pass to your baby through breast milk. However, many are considered safe, and your doctor can guide you on the best option based on your symptoms and nursing status.
Postpartum depression affects up to 15% of individuals. It involves emotional highs and lows, frequent crying, fatigue, guilt, anxiety, and challenges in caring for the baby. If you’re experiencing postpartum depression, remember you’re not alone. It’s not your fault, and help is available.
Top 5 Postpartum Depression Medications
Although various medications, typically antidepressants, are commonly used to treat postpartum depression (PPD), only one is FDA-approved for the condition. Despite the challenge of seeking help, treating PPD is crucial for both your well-being and that of your new baby.
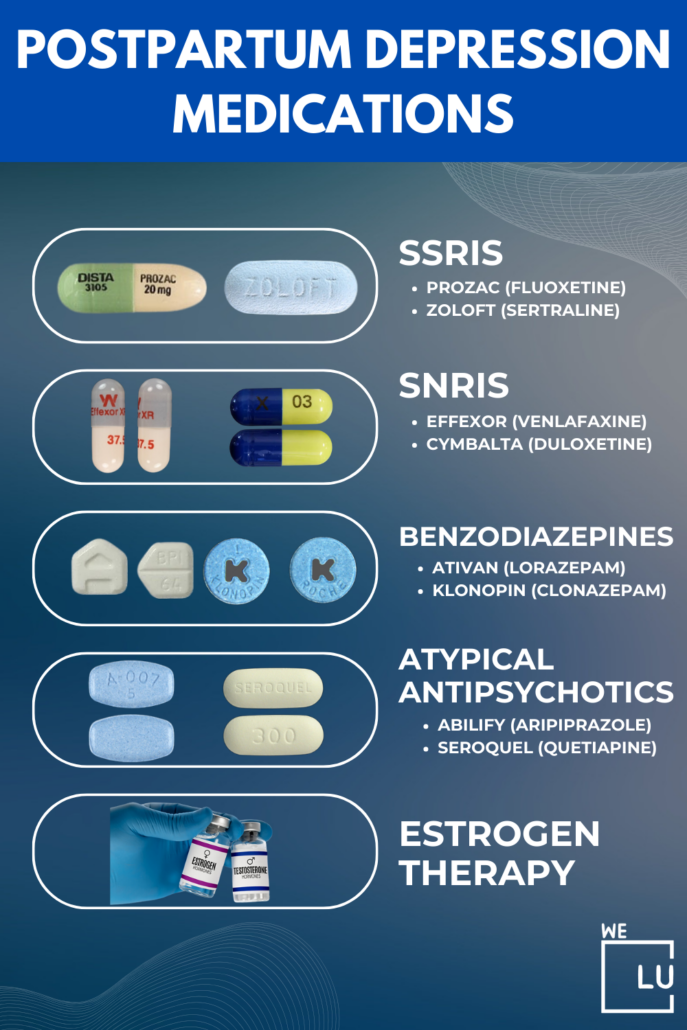
1. Selective Serotonin Reuptake Inhibitors (SSRIs)
The FDA-approved postpartum drugs belong to selective serotonin reuptake inhibitors (SSRIs). SSRIs are antidepressants that boost serotonin levels in the brain, a neurotransmitter linked to mood regulation. This mechanism makes SSRIs a helpful choice for easing symptoms of depression, including postpartum depression.
SSRIs are considered a first-line treatment for postpartum depression due to their effectiveness and safety profile. These medications not only help improve mood but also address associated symptoms such as fatigue, guilt, and anxiety.
Common SSRI medications are:
- Fluoxetine (Prozac): Prozac is a well-known SSRI that has been used for years to treat various depressive disorders. It works by inhibiting serotonin reuptake, allowing it to remain in the brain longer and positively impacting mood.
- Sertraline (Zoloft): Zoloft is another widely prescribed SSRI. It is known for its effectiveness in treating depression and anxiety, making it a common choice for postpartum depression. Sertraline works by increasing serotonin levels promoting emotional stability.
- Escitalopram (Lexapro): Lexapro is a newer SSRI that is often favored for its relatively mild side effects. It targets serotonin reuptake, helping to rebalance neurotransmitter levels and alleviate symptoms of depression.
When you begin an SSRI, it might take 3 to 4 weeks or more for symptoms to improve. If it works, you must take it for six months to 1 year. If symptoms don’t return, your provider may suggest gradually reducing the dose and stopping the medication. SSRIs usually have few long-lasting side effects, except for possible lingering sexual side effects if they occur.
While SSRIs can be highly beneficial, the decision to use them should be made in consultation with a healthcare provider, considering factors such as breastfeeding and individual health history.
2. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs show promise in treating postpartum depression with a dual action on mood regulation. SNRIs are antidepressants that, similar to SSRIs, impact brain neurotransmitters. They mainly focus on serotonin and norepinephrine, chemicals linked to mood. By preventing their reuptake, SNRIs maintain higher levels, enhancing mood.
SNRIs are seen as a helpful option for treating postpartum depression because they work on both serotonin and norepinephrine, providing a broader range of mood regulation. This dual effect may offer relief from various symptoms linked to postpartum depression.
Common SNRI medications are:
- Venlafaxine (Effexor): Effexor is a widely prescribed SNRI known for its dual action on serotonin and norepinephrine. It has been utilized to treat various mood disorders, including postpartum depression.
- Duloxetine (Cymbalta): Cymbalta is another commonly prescribed SNRI affecting serotonin and norepinephrine levels. It is often chosen for its efficacy in managing not only depression but also anxiety and chronic pain conditions.
- Desvenlafaxine (Pristiq): Pristiq is a newer SNRI that is an active metabolite of venlafaxine. It is often prescribed for its effectiveness in treating depressive symptoms and is considered a viable option for postpartum depression.
SNRIs share side effects with SSRIs, but they may cause more nausea, sleep issues, dry mouth, and changes in blood pressure. Similar to SSRIs, these side effects typically diminish over time.
3. Wellbutrin for Postpartum Depression
Wellbutrin, or bupropion, is an antidepressant explored as a potential treatment for postpartum depression (PPD). Unlike typical SSRIs and SNRIs for PPD, Wellbutrin mainly affects dopamine and norepinephrine. Some studies suggest it might be a suitable option, especially for those not responding well to other antidepressants.
For individuals thinking about Wellbutrin for postpartum depression, it’s crucial to consult their healthcare provider. The decision to use Wellbutrin, considering factors like individual health and breastfeeding, should be based on a thorough assessment. Open communication with a healthcare professional helps determine the most fitting treatment plan for the specific needs of the individual experiencing postpartum depression.
Bupropion has side effects similar to SSRIs and SNRIs but is less likely to cause sexual problems.
4. Nortriptyline Medication for Postpartum Depression
Nortriptyline, a tricyclic antidepressant (TCA), is commonly used to treat depression. It affects various chemical messengers in the central nervous system, focusing mainly on norepinephrine and serotonin.
A 2006 study found that nortriptyline, when used for postpartum depression (PPD), led to similar improvements in symptoms as sertraline. Some evidence suggests it may be as effective as SSRIs or psychotherapy for PPD. However, TCAs like nortriptyline typically cause more side effects, such as dry mouth, blurred vision, and drowsiness, making them not the first-choice treatment for depression.
Skip To:
Learn More:
- How Long Does Postpartum Depression Last?
- Postpartum Depression Treatment, Causes, Symptoms, Anxiety in Pregnancy, and Risks
- Learn How to Cope with Depression. 10 Ways to Cope with Depression.
- Understanding Postpartum Anxiety. Guide To The Postpartum Anxiety Symptoms, Causes, Diagnosis, and Treatment
- Are There Stages of Depression? Understanding Symptoms, Causes, and Effective Treatments
- What is Mild Depression? Symptoms and Treatment
- What is Crippling Depression? Learning How To Deal With Crippling Depression
- Signs of Depression in Women To Watch Out For. Comparing Depression in Men Vs. Women. What are the Causes of Depression in Women?
- Atypical Depression. What Is It? Symptoms and Treatment
- Guide to Situational Depression Symptoms, Causes, and Effective Treatment
5. Zulresso Postpartum Depression Medicine
In 2019, the FDA approved Zulresso (brexanolone) as the first and only medication specifically for postpartum depression (PPD). It is an option for individuals diagnosed with PPD who are at least 15 years old and do not have severe kidney disease.
Zulresso, a synthetic form of allopregnanolone, a hormone-related molecule, is administered through IV infusion over 2.5 days in a particular treatment center. It works by replenishing allopregnanolone levels in the body, potentially impacting the GABA system in the brain associated with mood.
Unlike traditional antidepressants, Zulresso takes just three days to show effects, but it comes with a higher cost and requires 24-hour monitoring due to potential sedation and other side effects. Despite these considerations, Zulresso has demonstrated effectiveness in clinical trials, leading to its breakthrough therapy status and rapid FDA approval.
We Level Up FL Mental Health Treatment Center Tips In Choosing Postpartum Depression Medication
✅ When selecting postpartum depression medication, consult with your healthcare provider or a mental health professional to discuss options tailored to your needs.
✅ Consider factors such as potential side effects, your health history, and if you are breastfeeding.
✅ It’s essential to choose a medication that is both effective for treating postpartum depression and suitable for your circumstances.
Get postpartum depression medication and counseling that works. Discover professional help from We Level Up Florida’s mental health therapists. Start getting support with a free call to our mental health hotline.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Dual Diagnosis Mental Health Centers Near You?
Even if therapy failed previously, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about counseling alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
FREE 24/7 Dual Diagnosis Mental Health Services HotlineIs Talk Therapy Effective for Postpartum Depression?
Talk therapy can be highly effective for postpartum depression. Engaging in therapy sessions provides a supportive environment where individuals can express their feelings, gain insights into their emotions, and develop coping strategies. The therapeutic process fosters a connection with a mental health professional who can offer guidance and support, contributing to the overall treatment and recovery from postpartum depression.
The most common psychotherapies for postpartum depression include the following:
- Cognitive Behavioral Therapy (CBT): CBT talk therapy helps individuals identify and change negative thought patterns and behaviors, promoting healthier coping mechanisms.
- Interpersonal Therapy (IPT): IPT focuses on improving interpersonal relationships and communication skills and addressing issues that may contribute to postpartum depression.
- Supportive Psychotherapy: This therapy provides emotional support and guidance, allowing individuals to discuss their feelings and concerns in a safe and empathetic environment.
- Mindfulness-Based Therapy: Mindfulness techniques, such as meditation and deep breathing, are incorporated to help individuals manage stress and stay present in the moment.
- Psychodynamic Therapy: Exploring unconscious thoughts and emotions, psychodynamic therapy aims to uncover and address underlying issues contributing to postpartum depression.
- Group Therapy: Group settings offer a supportive community where individuals can share experiences, receive feedback, and gain insights from others going through similar challenges.
The choice of psychotherapy depends on individual preferences, the severity of symptoms, and the specific needs of the person experiencing postpartum depression. Working with a mental health professional to determine the most appropriate therapeutic approach is essential.
Lifestyle and Home Remedies for Postpartum Depression
Several lifestyle and home remedies may help manage postpartum depression. Here are some things you can try:
- Social Support: Surround yourself with a supportive network of family and friends. Share your feelings and experiences to alleviate the emotional burden.
- Regular Exercise: Engage in light exercises like walking or yoga to boost mood-enhancing endorphins and improve overall well-being.
- Adequate Sleep: Prioritize getting enough rest by creating a consistent sleep schedule. Lack of sleep can exacerbate symptoms of postpartum depression.
- Healthy Nutrition: Maintain a balanced diet with nutritious foods to support your physical and mental health.
- Time for Yourself: Allocate moments for self-care activities that bring you joy and relaxation. It could be reading, taking a bath, or pursuing a hobby.
- Set Realistic Expectations: Avoid placing excessive pressure on yourself. Set achievable goals and be kind to yourself if things don’t go as planned.
- Limit Stressors: Identify and reduce sources of stress in your life. Delegate tasks when possible and focus on activities that bring a sense of calm.
- Mindfulness and Relaxation Techniques: Practice mindfulness, meditation, or deep-breathing exercises to manage stress and promote peace.
- Limit Alcohol and Caffeine: Excessive alcohol and caffeine intake can affect mood. Moderation is vital in maintaining emotional balance.
- Professional Help: Don’t hesitate to seek help from mental health professionals, such as therapists or counselors, who specialize in postpartum depression.
It’s essential to consult with a mental health professional before making significant lifestyle changes or starting new remedies to ensure they suit your circumstances.
Do you have questions about postpartum depression medication or treatment in general? Call our helpline 24/7.

End the Emotional Pain. Get Your Life Back.
Feeling Depressed, Anxious or Struggling with Mental Health Illness? Get Safe Comfortable Mental Health Dual Diagnosis High-Quality Therapy From Counselors That Care. Begin Your Recovery Now.
Hotline (855) 940-6125How is Postpartum Depression Diagnosed?
Healthcare providers, such as obstetricians, gynecologists, or mental health specialists, diagnose postpartum depression through a thorough assessment. During postpartum check-ups, professionals ask about the new mother’s emotional well-being and use standardized questionnaires to evaluate depressive symptoms like mood changes, sleep patterns, energy levels, and appetite shifts. Open communication about feelings and experiences is crucial for an accurate diagnosis.
In some cases, additional screenings or referrals to mental health specialists may be done for a more detailed evaluation. The diagnostic process considers symptoms’ duration, intensity, and impact on daily life.
What Causes Postpartum Depression?
Several risk factors contribute to the development of postpartum depression (PPD). While individual experiences vary, here is a list of common risk factors:
- Previous History of Depression: A history of depression or mental health issues, whether during pregnancy or at other times in life, increases the risk of postpartum depression.
- Personal or Family History of Mental Health Disorders: A family history of mood disorders, including depression or bipolar disorder, can elevate the risk.
- Lack of Social Support: Limited support from family, friends, or a partner may contribute to feelings of isolation, increasing the likelihood of postpartum depression.
- High Stress Levels: High stress, whether related to pregnancy, childbirth, or external factors, can increase vulnerability to postpartum depression.
- Complications During Pregnancy or Birth: Difficulties during pregnancy or childbirth, such as complications or traumatic experiences, can contribute to postpartum depression.
- Hormonal Changes: Fluctuations in hormonal levels, particularly a rapid drop in estrogen and progesterone after childbirth, may play a role in the development of postpartum depression.
- Unplanned or Unwanted Pregnancy: Feelings of being unprepared or having an unplanned or unwanted pregnancy can contribute to the risk of postpartum depression.
- Financial Strain: Economic challenges or financial stressors can impact mental health during the postpartum period.
- Marital or Relationship Issues: Strained relationships or lack of support from a partner can be a risk factor for postpartum depression.
- Sleep Deprivation: Disrupted sleep patterns, common in the early postpartum period, may contribute to increased vulnerability to depression.
The presence of these risk factors doesn’t guarantee the development of postpartum depression, and individuals without these factors may still experience PPD. The interplay of various factors is complex, and each person’s experience is unique.
How Long Does Postpartum Depression Usually Last?
Postpartum depression (PPD) can last different amounts of time for each person. Symptoms often start in the first few weeks after childbirth and may continue for several months. Without treatment, PPD might last a year or more for some individuals. However, getting help early and starting treatment can speed up recovery.
The duration depends on individual factors, the symptoms’ severity, and how well the treatment works. Seeking professional help, like therapy or postpartum depression medication, can help resolve postpartum depression symptoms more quickly.
First-class Facilities & Amenities
World-class High-Quality Mental Health Services & Behavioral Health Substance Abuse Treatment
Rehab Centers TourRenowned Mental Health Centers. Serene Private Facilities. Inpatient Rehab Programs Vary.
Mental Health Helpline (855) 940-6125Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Successes
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Development Events
- Comfortable Onsite Medical Detox Center
Postpartum Psychosis Treatment
Postpartum psychosis is a rare but severe mental health condition that can happen after childbirth. It involves quick-onset symptoms like hallucinations, delusions, and intense mood swings. Immediate medical attention is vital for the safety of both the mother and the infant.
Treatment usually includes medication, therapy, and hospitalization.
- Antipsychotic prescriptions are often used to manage symptoms, and sometimes mood stabilizers are recommended.
- Hospitalization ensures the safety of both the mother and the baby because postpartum psychosis can lead to severe and unpredictable behavior. In the hospital, the mother gets constant monitoring, support, and a structured environment to stabilize.
- Therapies like cognitive-behavioral therapy or psychodynamic therapy may be used to address underlying issues and provide coping strategies.
If there are concerns about postpartum psychosis, it’s crucial to seek immediate medical attention because quick and appropriate treatment dramatically improves outcomes.
What Happens If Postpartum Depression Isn’t Treated?
If postpartum depression isn’t treated, it can have lasting effects on both the mother and the baby. The mother may continue to feel sad, hopeless, and anxious, making it harder to connect with and care for the baby. Untreated postpartum depression can strain relationships, disrupt family life, and lead to ongoing mental health challenges for the mother. The baby may also be affected, as the mother’s emotional well-being is crucial for building a secure and healthy attachment.
Early intervention and proper treatment are essential to lessen the potential long-term impact of untreated postpartum depression on both the mother’s and the baby’s well-being.
Suppose you or someone you know has postpartum depression, which affects their daily functioning. In that case, We Level Up Florida Mental Health Treatment Center provides personalized care with a team of experienced professionals. Begin your journey towards better health by taking the first step towards healing. Get help. Call We Level Up FL now. Each call is free and confidential.
World-class, Accredited, 5-Star Reviewed, Effective Mental Health Dual Diagnosis Programs. Complete Integrated Inpatient Rehab with Free Post Discharge Therapy Planning.
CALL (855) 940-6125End the Emotional Pain Rollercoaster. Gain Stability & Happiness Through Recovery Treatment. Start Mental Health Counseling Today. Get Free No-obligation Guidance by Behaviroal Health Specialists Who Understand Mental Health Recovery.
Therapist Tips to Cope and Combat Depressive Episodes
Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.



Start a New Life
Begin with a free call to a behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
Search We Level Up FL Postpartum Depression Medication, Mental Health Topics & Resources
Sources
- Mughal S, Azhar Y, Siddiqui W. Postpartum Depression. [Updated 2022 Oct 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519070/
- Frieder A, Fersh M, Hainline R, Deligiannidis KM. Pharmacotherapy of Postpartum Depression: Current Approaches and Novel Drug Development. CNS Drugs. 2019 Mar;33(3):265-282. Doi: 10.1007/s40263-019-00605-7. PMID: 30790145; PMCID: PMC6424603.
- Suryawanshi O 4th, Pajai S. A Comprehensive Review on Postpartum Depression Medication. Cureus. 2022 Dec 20;14(12):e32745. Doi: 10.7759/cureus.32745. PMID: 36686097; PMCID: PMC9851410.
- Postpartum depression – Office on Women’s Health (.gov)
- FDA Approves First Oral Treatment for Postpartum Depression – Food and Drug Administration (.gov)
- Fitelson E, Kim S, Baker AS, Leight K. Treatment of postpartum depression: clinical, psychological and pharmacological options. Int J Womens Health. 2010 Dec 30;3:1-14. Doi: 10.2147/IJWH.S6938. PMID: 21339932; PMCID: PMC3039003.
- Depression Among Women – Centers for Disease Control and Prevention (CDC)
- Depression During and After Pregnancy – Centers for Disease Control and Prevention (CDC)
- Treating Postpartum Depression – Whole Health Library – Veterans Affairs (.gov)
- Postpartum Depression – MedlinePlus (.gov)