Anxiety in Pregnancy & Postpartum Depression Treatment
First-line treatment for postpartum depression and anxiety in pregnancy treatment is psychotherapy and antidepressant medications. Antidepressants, in general, are considered to be anxiety meds safe for pregnancy and relatively safe for use during breastfeeding when clinically warranted, and SSRIs in particular are one of the best-studied classes of medications during breastfeeding.
Psychosocial and psychological psychotherapy is the first-line treatment option for women with mild to moderate peripartum and postpartum depression, especially if mothers are hesitant about starting on medications and are going to nurse the newborn. A combination of therapy and antidepressant drugs is recommended for women with moderate to severe depression and anxiety during pregnancy. Selective serotonin reuptake inhibitors (SSRIs) are the first choice as safe anxiety medications during pregnancy. Consider switching to serotonin-norepinephrine reuptake inhibitors (SNRIs) or mirtazapine if SSRI is ineffective. Once an effective anxiety medication pregnancy dose is reached, continue anxiety medication during pregnancy treatment for 6 to 12 months to prevent relapse of symptoms.
Pharmacologic depression and anxiety medication safe in pregnancy recommendations for women who are lactating should include discussing the benefits of breastfeeding, the risks of antidepressant use during lactation, and the risks of untreated illness. Repetitive transcranial magnetic stimulation (TMS) is a treatment that may provide an alternative depression and anxiety medication for pregnancy option for women who breastfeed and are concerned about their babies being exposed to medication.
Patients with severe postpartum depression and early pregnancy anxiety symptoms may not respond to psychotherapy and pharmacotherapy. For patients with severe postpartum depression and pregnancy paranoia anxiety that decline or do not respond to electroconvulsive therapy, intravenous Brexanolone is recommended. Brexanolone received FDA approval in March 2019, and it is the first drug to be specifically approved for postpartum depression. [1]
What is Postpartum Depression?
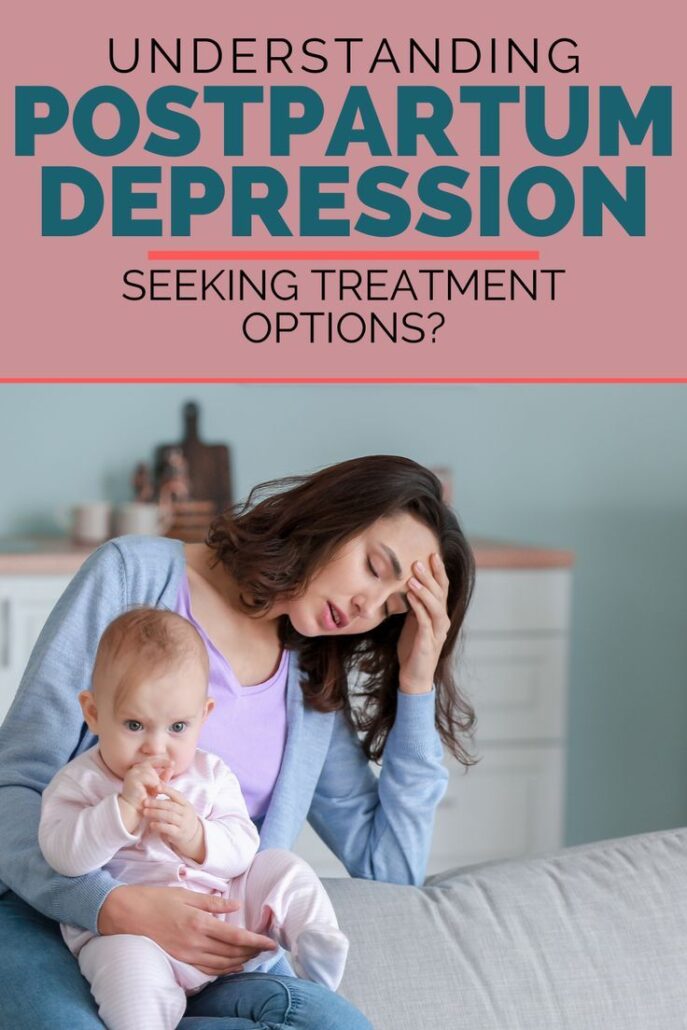
Known as “baby blues,” postpartum depression (PPD) is moderate to severe depression in a woman after she has given birth. Thus, it may occur soon after delivery or up to a year later. Most of the time, it occurs within the first 3 months after delivery. Without a doubt, it is a real mental health condition that requires proper diagnosis and postpartum depression treatment.
Untreated postpartum depression is not only a problem for the mother’s health and quality of life, but can affect the well-being of the baby. This is according to the National Center for Biotechnology Information. [2]
A woman’s hormones change after childbirth. Insomnia contributes to stress and anxiety after pregnancy. Some depression and sadness after giving birth are normal, but if they persist for more than a few weeks, postpartum depression may be present. The levels of two hormones, estrogen, and progesterone, drop very quickly after a new mom gives birth. Thus, this change triggers mood swings.
Those who present with mild depression and anxiety about pregnancy symptoms often don’t get help. This can happen because they do not realize that what they’re experiencing is a real condition, or they may not connect their feelings with the childbirth experience. Postpartum depression and anxiety during pregnancy third trimester can be serious. Untreated, it may lead to long-lasting or recurring depressive symptoms.
Motherhood brings in a variety of challenges that could impact both the mother and her family. Getting help for postpartum depression and anxiety in early pregnancy symptoms may seem difficult. However, it’s important to know that treatment for postpartum depression and anxiety medication safe for pregnancy are available.
Causes of Postpartum Depression & End of Pregnancy Anxiety
- Fluctuations in hormone level
- History of mood disorders. Examples are major depression and bipolar disorder.
- Lack of sleep
- Being under 25 years old
- Current alcohol or drug use
- Having an unplanned pregnancy, or experiencing mixed feelings about pregnancy
- Experiencing a stressful life event during pregnancy or delivery
- Having a close relative with depression, anxiety, or other mental illness
- Poor relationship with a partner, or no partner
- Lower socioeconomic status can contribute to financial or housing issues
- Lacking social and/or emotional support
- History of substance use
List of Anxiety Medications Safe During Pregnancy
It is important that physicians understand the course of these disorders during pregnancy and available treatments for anxiety and depression in pregnancy. It will help them appropriately counsel women who are or intend to become pregnant. The goal of treatment during pregnancy and lactation is sufficient treatment for syndrome remission. To minimize the potential for neonatal withdrawal and maternal toxicity after delivery, vigilant monitoring of side effects is indicated. Also, if possible, nonpharmacologic treatment, such as cognitive-behavioral therapy, should be the first-line treatment in pregnant women with a generalized anxiety disorder or panic disorder.
The FDA also urges women not to use marijuana or any type of CBD product while pregnant or breastfeeding. It could be dangerous for you and your baby. It may cause CBD pregnancy anxiety induced and worsen over time.
Some of the anxiety medication and pregnancy depression treatments that are safe include Selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) are first-choice anxiety medications during pregnancy.
SSRIs are a common group of medications used to treat anxiety. Examples of SSRIs anxiety meds for pregnancy include:
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
Skip To:
Learn More:
Postpartum Depression Fact Sheet
Postpartum Depression Overview
“Postpartum” means the time after childbirth. Most women get the “baby blues,” or feel sad or empty, within a few days of giving birth. For many women, the baby blues go away in 3 to 5 days. If your baby blues don’t go away or you feel sad, hopeless, or empty for longer than 2 weeks, you may have postpartum depression. Feeling hopeless or empty after childbirth is not a regular or expected part of being a mother.
Postpartum depression is a serious mental illness that involves the brain and affects your behavior and physical health. If you have depression, then sad, flat, or empty feelings don’t go away and can interfere with your day-to-day life. You might feel unconnected to your baby, as if you are not the baby’s mother, or you might not love or care for the baby. These feelings can be mild to severe.
Epidemiology of Postpartum Depression
Postpartum depression most commonly occurs within 6 weeks after childbirth. PPD occurs in about 6.5% to 20% of women. It occurs more commonly in adolescent females, mothers who deliver premature infants, and women living in urban areas. African American and Hispanic mothers reported the onset of symptoms within 2 weeks of delivery, unlike white mothers, who reported the onset of symptoms later, as one study reports.
Risk Factors of Postpartum Depression
Psychological: History of depression and anxiety, premenstrual syndrome (PMS), Negative attitude towards the baby, the reluctance of baby’s gender, and history of sexual abuse are perpetual factors for developing postpartum depression.
Obstetric risk factors: Risky pregnancy, which includes emergency cesarean section and hospitalizations during pregnancy. Meconium passage, umbilical cord prolapse, preterm or low birth infant, and low hemoglobin are associated with PPD.
Social factors: Lack of social support can cause postpartum depression. Domestic violence in the form of spousal sexual and physical, and verbal abuse can also be a causative factor in the development of the disease. Smoking during pregnancy is a risk factor for developing PPD.
Lifestyle: Eating habits, sleep cycle, physical activities, and exercise may affect postpartum depression. Vitamin B6 has known to be involved in postpartum depression via its conversion to tryptophan and, later on, serotonin, which, in turn, affects mood. The sleep cycle is among the factors influencing the risk of depression. It is evident that decreased sleep is associated with postpartum depression. Physical activity and exercise decrease depressive symptoms.PPD.
Although less studied than depression, research on anxiety attacks during pregnancy effects on baby suggests that anxiety may negatively affect both the mother and the fetus. Anxiety increases the risk for preterm birth, low birthweight, earlier gestational age, and a smaller head circumference (which is related to brain size).
Postpartum Depression Statistics
Depression is a common and serious illness. A CDC study shows that about 1 in 10 women in the United States reported symptoms that suggest they experienced an episode of major depression in the last year. While exact postpartum depression rates are unknown, there are some generally agreed-upon figures about the number of women who experience postpartum depression annually.
1 in 10 Women
Approximately 1 in 10 women will experience postpartum depression after giving birth, with some studies reporting 1 in 7 women.
Source: National Institute on Mental Health
3 to 6 Months
Postpartum depression generally lasts 3 to 6 months, however, this varies based on several factors.
Source: National Institute on Mental Health
50%
It is estimated that nearly 50% of mothers with postpartum depression are not diagnosed by a health professional.
Source: National Institute of Mental Health
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Dual Diagnosis Mental Health Centers Near You?
Even if therapy failed previously, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about counseling alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
FREE 24/7 Dual Diagnosis Mental Health Services HotlinePostpartum Depression Symptoms
Postpartum depression affects each individual differently and to a different degree. Some women experience rare but extreme cases of the condition known as postpartum psychosis. On the other hand, some women experience a milder and more short-term type called “baby blues.”
“Baby blues” are often the result of hormonal changes right after birth. Right after the baby is born, new moms will experience a sudden dip in hormone levels (specifically estrogen and progesterone) which can cause depression symptoms.
During postpartum depression—also known as perinatal depression—women most commonly experience emotional symptoms that affect how they feel. These emotional symptoms include:
- Depression
- Loss of interest in activities once enjoyed
- Changes in appetite
- Trouble sleeping or sleeping too much
- Increase in fatigue
- Feeling worthless
- Difficulty thinking or making decisions
- Thoughts of death or suicide
- Crying for “no reason”
- Lack of interest in the baby, not feeling bonded to the baby, or feeling very anxious about/around the baby
- Feelings of being a bad mother
- Lack of interest in the baby, not feeling bonded to the baby, or feeling very anxious about/around the baby

End the Emotional Pain. Get Your Life Back.
Feeling Depressed, Anxious or Struggling with Mental Health Illness? Get Safe Comfortable Mental Health Dual Diagnosis High-Quality Therapy From Counselors That Care. Begin Your Recovery Now.
Hotline (855) 940-6125Postpartum Depression Treatments
Treatment for postpartum depression and recovery time varies, depending on the severity of your depression and your individual needs. Postpartum depression (PPD) refers to a spectrum of illnesses experienced by some women after childbirth. Postpartum psychosis may occur when severe mood changes are accompanied by delusions or hallucinations, which may require hospitalization for treatment. Postpartum psychosis can be life-threatening for both the woman and her baby if it’s not recognized and treated early.
People with postpartum depression also report having these self-critical thoughts: “I’m not cut out for this.” “Something’s wrong with me.” PPD is more than just feeling sad, irritable, or overwhelmed by new motherhood. It is time to seek help, and postpartum depression treatment, if the feelings won’t go away or if they get worse.
Postpartum depression treatment starts with a diagnosis of postpartum depression based on your symptoms and your medical and pregnancy history. It may help to talk through your concerns with a psychiatrist, psychologist, or other mental health professionals.
Set realistic goals and respond to situations in a positive way. Postpartum depression should be diagnosed and treated promptly because it can affect you and your baby. Postpartum depression usually lasts from a few days to several weeks after delivery, and during treatment for postpartum depression, your doctor may recommend an antidepressant.
With proper postpartum depression treatments, the symptoms of PPD usually improve, it is important, too, to have real emotional support from friends, family, or your maternity team.
Benefits of Postpartum Depression Treatments
Once individuals have been diagnosed with PPD, they can pursue a variety of treatments for postpartum depression options to help them achieve a healthy mind and body. Antidepressants are central to treating depression and anxiety during pregnancy. but it is crucial to weigh the risks and benefits with your health care provider, discuss all your symptoms to get a more personalized treatment as every mental health case is unique person to person.
First-class Facilities & Amenities
World-class High-Quality Mental Health Services & Behavioral Health Substance Abuse Treatment
Rehab Centers TourRenowned Mental Health Centers. Serene Private Facilities. Inpatient Rehab Programs Vary.
Mental Health Helpline (855) 940-6125Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Successes
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Development Events
- Comfortable Onsite Medical Detox Center
Cognitive Behavioral Therapy (CBT) for Postpartum Depression Treatment
Cognitive behavioral therapy has been shown to be an effective treatment for a variety of mental health problems in pregnancy including depression. anxiety. panic attacks.
- It has been proven to be significantly effective in treating PPD
- Involves identifying, understanding, and changing thinking and behavioral patterns to help individuals change the way they feel
- Provides a hands-on, practical approach to problem-solving
- CBT helps individuals:
- Learn to control their thinking
- Maintain a sense of control and self-confidence
- Learn lifelong coping skills
Interpersonal Therapy for Postpartum Depression Treatment
- Addresses interpersonal issues influencing depression
- This entails gathering information about the nature of a person’s depression and interpersonal experience
- Involves 12 to 16 hours of weekly sessions
Group Therapy for Postpartum Depression Treatment
- Draws upon a variety of cognitive-behavioral techniques, such as mindfulness, to help individuals develop skills for:
- Regulating emotions
- Tolerating distress
- Managing relationships
Antidepressants for Postpartum Depression Treatment
- Medications affect the brain chemicals involved in mood regulation. A common class of antidepressants prescribed for PPD: is selective-reuptake inhibitors (SSRIs), such as fluoxetine and sertraline.

World-class, Accredited, 5-Star Reviewed, Effective Mental Health Dual Diagnosis Programs. Complete Integrated Inpatient Rehab with Free Post Discharge Therapy Planning.
CALL (855) 940-6125End the Emotional Pain Rollercoaster. Gain Stability & Happiness Through Recovery Treatment. Start Mental Health Counseling Today. Get Free No-obligation Guidance by Behaviroal Health Specialists Who Understand Mental Health Recovery.
7 Tips for a Healthier Lifestyle after Postpartum Depression Treatment
- Incorporate exercise into your daily routine
- Maintain a healthy diet and avoid alcohol
- Set manageable expectations for daily activities
- Build new relationships and foster existing ones
- Discuss your feelings and experiences with family and friends
- Don’t be ashamed to ask for or accept help from others
- Seek advice about parenting from trusted individuals
Postpartum Depression Natural Treatment
Both our physical health and our mental health are greatly influenced by what we eat. Ensuring that you get enough nutrients is important in postpartum depression treatment. Some that have been found to be particularly beneficial after childbirth includes, but aren’t limited to:
- Omega-3 fatty acids
- B vitamins, especially vitamins B6 (riboflavin) and B12 (folate)
- SAMe (a molecule found naturally in the body that is also produced as a supplement)
In addition to nutrition and lifestyle, you can help overcome PPD in a variety of other ways. One popular and effective natural treatment for postpartum depression is bright light therapy. It’s safe and easy to use. Sitting in front of a lightbox for as little as a half hour per day can stimulate your brain in ways that reduce depression.
How Long Does Postpartum Depression Last?
The postpartum period generally includes the first 4–6 weeks after birth, and many cases of PPD begin during that time. But PPD can also develop during pregnancy and up to 1 year after giving birth.
The Postpartum Period (PPD) is typically divided into four distinct stages: prenatal, perinatal, early postpartum, and late postpartum. The prenatal stage covers the pregnant woman’s entire pregnancy and extends through her delivery and the initial recovery period following childbirth. The perinatal stage begins with delivery and ends 7 days later with a visit from a healthcare provider who determines whether or not there are signs of serious maternal or infant problems.
The early postpartum period lasts from 7 days after birth to 6 weeks following childbirth. The late postpartum period begins at 6 weeks and continues for up to 1 year, or until the woman’s body completely returns to its non-pregnant state. Postpartum depression can occur during any of these stages, but it most often begins in the first few months after delivery.
Postpartum Depression (PPD) is a type of clinical depression that can affect both sexes after childbirth, though it occurs more frequently in females than males. Postpartum depression can cause sadness, fatigue, anxiety, weight changes, and trouble sleeping and concentrating. Postpartum Depression affects about 15-20% of mothers within the first three months.
Postpartum Depression Treatment Facility and Co-Occurring Issues

When a woman is suffering from postpartum depression, she may be more likely to self-medicate. Also, women may experience symptoms of anxiety. One study found that nearly two-thirds of women with postpartum depression also experience an anxiety disorder. Postpartum depression treatment can be necessary for cases suffering from deep depression.
Where there are co-occurring multiple disorders postpartum depression treatment requires more sophisticated specialists able to recognize and treat the entire of all the disorders for long-term recovery. Mothers who develop postpartum depression may be less likely to seek treatment of postpartum depression. This is because many women are embarrassed to admit that they are suffering from severe postpartum depression. Thankfully, this is starting to change as there is now greater awareness and understanding of this condition.
According to SAMHSA (Substance Abuse and Mental Health Service Administration), as many as 15% of women suffering from postpartum depression engage in binge drinking within a year of giving birth. Women battling postpartum depression who drink to cope greatly increase the risk of exposing their children to alcohol poisoning. Hence, alcohol can pass from mother to child during breastfeeding and studies have shown that this can stunt a baby’s growth.
We Level Up mental health center has trained counselors that are qualified to provide postpartum depression treatment. Lean on us to get the help you deserve to care for you and your baby. Searching for postpartum depression treatment near me? Call to learn more about postpartum depression treatment options suitable for your circumstances.
Top 5 Depression Anxiety and Pregnancy FAQs
-
Is anxiety a symptom of pregnancy? Is anxiety a sign of pregnancy?
Hormonal changes, exhaustion, and stress can all cause mood swings in early pregnancy. It is common to have greater emotional sensitivity and mood swings throughout pregnancy. Pregnancy can also result in relapses of pre-existing mental health problems including despair and anxiety.
-
Can pregnancy cause anxiety? Does pregnancy cause anxiety?
Have you ever wondered why you’re having pregnancy anxiety at night? Antenatal anxiety is another term for anxiety around pregnancy. Anxiety attack pregnancy symptoms are common and can affect any parent. If you experience pregnancy scare anxiety, you may be concerned about your baby’s health and development, and you may require regular reassurance that they are healthy and developing correctly.
-
Can pregnancy hormones cause anxiety and depression?
Hormone changes during pregnancy can influence brain chemistry, causing depression in pregnancy and anxiety. Pregnant women may be unaware that they are depressed or having anxiety early pregnancy symptoms. They may believe they are experiencing pregnancy symptoms or the “baby blues,” which many women experience immediately after giving birth.
-
How to treat pregnancy after miscarriage anxiety? Treating early pregnancy anxiety about miscarriage.
Talk about your feelings and allow yourself to experience them fully. Turn to your partner, family, and friends for comfort. If this still feels too overwhelming, break your time down further – focus on getting through just one day at a time. If you’re having trouble coping with an anxiety pregnancy symptom early indication, consult your healthcare provider or a counselor for extra support.
-
What to do when you have anxiety during pregnancy second trimester?
Anxiety chest pain during pregnancy and other signs of anxiety and pregnancy should be treated with therapy. You may also choose to explore safe anxiety meds during pregnancy, particularly if anxiety has a significant impact on your life or if treatment alone is ineffective. Spending time for self-care, participating in support groups, and utilizing community services can also assist with anxiety.
Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.



Start a New Life
Begin with a free call to a behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
Search We Level Up FL Postpartum Depression Treatment, Mental Health Topics & Resources
Sources
[1] Mughal S, Azhar Y, Siddiqui W. Postpartum Depression. [Updated 2022 Oct 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519070/
[2] Fitelson E, Kim S, Baker AS, Leight K. Treatment of postpartum depression: clinical, psychological and pharmacological options. Int J Womens Health. 2010 Dec 30;3:1-14. DOI: 10.2147/IJWH.S6938. PMID: 21339932; PMCID: PMC3039003.
SAMHSA (Substance Abuse and Mental Health Service Administration) – https://www.samhsa.gov/grants/grant-announcements/ti-14-005
[3] US Department of Health and Human Services – https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression/postpartum depression treatment near me
[4] NCBI – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6659987/treatment postpartum depression
[5] NIMH – https://www.nimh.nih.gov/health/topics/women-and-mental-healt
[6] OASH – https://www.womenshealth.gov/mental-health
[7] CDC – https://www.cdc.gov/reproductivehealth/depression/index.htm/treatment postpartum depression
[8] WHO – https://apps.who.int/iris/handle/10665/66539
[9] Postpartum Depression Treatment – https://welevelupnj.com/mental-health-services/postpartum-depression-treatment/
[10] Women’s Depression Treatment Center – https://welevelup.com/mental-health/womens-depression-treatment-center/