Criteria for Acute Stress Disorder
To uncover the difference between acute stress disorder vs PTSD, it’s crucial to understand that PTSD shares many of the same symptoms as Acute Stress Disorder. But the symptoms or effects of PTSD last a longer time than ASD.
Acute Stress Disorder (ASD) is a mental health problem that can occur in the first month after a traumatic event. The symptoms of ASD are like PTSD symptoms, but you must have them for longer than one month to have PTSD. [1]
Several factors can place you at higher risk for developing ASD after a trauma:
- Having gone through other traumatic events
- Having had PTSD or complex PTSD symptoms in the past
- Having had prior mental health problems
- Tending to have symptoms, such as not knowing who or where you are, when confronted with trauma
Acute stress disorder (ASD) was first outlined in 1994 in the diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV), as a new diagnosis. Searching for “acute stress disorder vs PTSD DSM 5?”
The reason for adding this diagnosis was to provide healthcare services to patients with acute traumas who were not covered by insurance due to the condition being in its early stage. Second, it was hoped to predict post-traumatic stress disorder (PTSD) development in acute trauma patients to initiate early interventions.
According to survey-based studies, twenty to ninety percent of the general population is exposed to one or more extreme stressful events in their life. Although many are exposed, only 1.3 to 11.2 percent of acute stress disorder (ASD) develop a long-term symptomatic disease (such as complex trauma or PTSD).
Acute stress disorder (ASD) is a psychiatric disorder. Still, it can have physiological manifestations (such as tachycardia) and abnormal fMRI (uses MR imaging to measure the tiny changes in blood flow that occur in an active part of the brain.)
However, no validated laboratory or radiographic test exists. The diagnosis is clinical and is based on history and physical examination. Careful behavior observation and careful listening to the patient’s narrative are of immense value. In the initial evaluation session, many patients cannot fully reflect on their feelings and history and will require additional visits. [2]
Skip To:
- Criteria for Acute Stress Disorder
- Acute Stress Disorder Checklist
- Acute Stress Disorder Prevalence
- Understanding PTSD
- PTSD Symptoms
- Difference Between Acute Stress Disorder and PTSD
- Similarities Between ASD and PTSD
- Acute Stress Disorder Vs PTSD
- Acute Stress Disorder Vs PTSD Treatment
Learn More:
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Dual Diagnosis Mental Health Centers Near You?
Even if therapy failed previously, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about counseling alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
FREE 24/7 Dual Diagnosis Mental Health Services HotlineAcute Stress Disorder Checklist
The diagnosis of ASD can only be considered from 3 days to one month following a traumatic event (commonly referred to as the acute phase). The main difference between PTSD and acute stress disorder is the duration of symptoms. If posttraumatic symptoms persist beyond a month, the clinician will assess for the presence of PTSD. The ASD diagnosis would no longer apply.
To diagnose ASD, a doctor may refer to the DSM-5 diagnostic criteria, the official diagnostic criteria listed by the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). [3] These are:
- Exposure to actual or threatened death, serious injury, or sexual violation: In addition to directly witnessing or experiencing a traumatic event, a person can be affected by ASD if they learn that a traumatic event happened to a close relative or friend or are exposed to traumatic events as part of their job.
- Presenting symptoms: Of the five categories of symptoms for ASD – intrusion, negative mood, dissociation, avoidance, and arousal – someone affected by ASD will present at least 9 of the 14 signs from any of the categories.
- Duration of the disturbance: The symptoms of ASD must last for at least three days for a diagnosis of ASD. They must also manifest between three days and one month after the traumatic event.
- Significant distress: The symptoms are debilitating enough to impact the person’s usual way of life, such as impaired performance at work or the inability to participate normally in social activities.
- Ruling out other causes: To diagnose ASD, the doctor must establish that a particular event is the root cause of the condition. They will, therefore, take care to identify any other possible causes, ruling out physical conditions, such as brain injury or other psychological conditions. They will also consider whether the condition could be attributed to the effects of substances such as medication or alcohol.

Acute Stress Disorder Prevalence
Studies of ASD vary in terms of the tools used and the rates of ASD found. Overall, within one month of trauma, survivors show rates of ASD ranging from 6% to 33%. Rates differ for different types of trauma. For example, survivors of accidents or disasters such as typhoons show lower rates of ASD. Survivors of violence such as robbery, assaults, and mass shootings show rates at the higher end of that range. [4]
For acute stress disorder vs adjustment disorder, adjustment disorder is typically triggered by a stressful event or phase but within the normal range of human experiences, such as a marriage breakup or financial difficulty. Conversely, ASD and PTSD are caused by an exceptional, traumatic event.

End the Emotional Pain. Get Your Life Back.
Feeling Depressed, Anxious or Struggling with Mental Health Illness? Get Safe Comfortable Mental Health Dual Diagnosis High-Quality Therapy From Counselors That Care. Begin Your Recovery Now.
Hotline (855) 940-6125Understanding PTSD
Post-traumatic stress disorder (PTSD) is a mental health disorder that some people develop after they experience or see a traumatic event. The traumatic event may be life-threatening, such as combat, a natural disaster, a car accident, or sexual assault. But sometimes, the event is not necessarily a dangerous one. For example, the sudden, unexpected death of a loved one can also cause PTSD.
It’s normal to feel afraid during and after a traumatic situation. The fear triggers a “fight-or-flight” response. This is your body’s way of helping to protect itself from possible harm. It causes changes in your body, such as the release of certain hormones and increases in alertness, blood pressure, heart rate, and breathing.
In time, most people recover from this naturally. But people with PTSD don’t feel better. They feel stressed and frightened long after the trauma is over. In some cases, PTSD triggers and symptoms may start later on. They might also come and go over time.
You can develop PTSD at any age. Many risk factors play a part in whether you will develop PTSD. [5] They include:
- Your sex; women are more likely to develop PTSD
- Having had trauma in childhood
- Feeling horror, helplessness, or extreme fear
- Going through a traumatic event that lasts a long time
- Having little or no social support after the event
- Dealing with extra stress after the event, such as the loss of a loved one, pain and injury, or loss of a job or home
- Having a history of mental illness or substance use
PTSD Symptoms
There are four types of PTSD symptoms, but they may not be the same for everyone. Each person experiences symptoms in their way. The types are:
- Re-experiencing symptoms, where something reminds you of the trauma, and you feel that fear again. Examples include:
- Flashbacks, which cause you to feel like you are going through the event again
- Nightmares
- Frightening thoughts
- Avoidance symptoms, where you try to avoid situations or people that trigger memories of the traumatic event. This may cause you to:
- Stay away from places, events, or objects that remind the traumatic experience. For example, if you were in a car accident, you might stop driving.
- Avoiding thoughts or feelings related to the traumatic event. For example, you might try to stay very busy to avoid thinking about what happened.
- Arousal and reactivity symptoms may cause you to be jittery or be on the lookout for danger. They include:
- Being easily startled
- Feeling tense or “on edge”
- Having difficulty sleeping
- Having angry outbursts
- Cognition and mood symptoms are negative changes in beliefs and feelings. They include:
- Trouble remembering important things about the traumatic event
- Negative thoughts about yourself or the world
- Feeling blame and guilt
- No longer being interested in things you enjoyed
- Trouble concentrating
The symptoms usually start soon after the traumatic event. But sometimes, they may not appear until months or years later. They also may come and go over many years. If your symptoms last longer than four weeks, cause you great distress, or interfere with your work or home life, you might have PTSD.
First-class Facilities & Amenities
World-class High-Quality Mental Health Services & Behavioral Health Substance Abuse Treatment
Rehab Centers TourRenowned Mental Health Centers. Serene Private Facilities. Inpatient Rehab Programs Vary.
Mental Health Helpline (855) 940-6125Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Successes
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Development Events
- Comfortable Onsite Medical Detox Center
Difference Between Acute Stress Disorder and PTSD
ASD is a risk factor for developing PTSD. However, not all individuals who meet the criteria for ASD will develop PTSD, and many individuals who develop PTSD do not first have an ASD diagnosis. Regardless of whether an individual develops PTSD, a diagnosis of ASD is important for individuals experiencing early significant distress in response to trauma to be identified and treated. [6]
ASD and PTSD share the same requirement for exposure to a traumatic event. Many of the ASD symptoms are similar to those of PTSD. Yet, ASD and PTSD differ in several important ways:
- PTSD diagnosis requires meeting a certain number of symptoms within established clusters. For ASD, symptoms are not classified within clusters; therefore, an individual meets diagnosis based upon the expression of symptoms in total.
- PTSD includes non-fear-based symptoms (i.e., risky or destructive behavior, overly negative thoughts and assumptions about oneself or the world, exaggerated blame of self or others for causing the trauma, negative affect, decreased interest in activities, and feeling isolated), whereas ASD does not.

World-class, Accredited, 5-Star Reviewed, Effective Mental Health Dual Diagnosis Programs. Complete Integrated Inpatient Rehab with Free Post Discharge Therapy Planning.
CALL (855) 940-6125End the Emotional Pain Rollercoaster. Gain Stability & Happiness Through Recovery Treatment. Start Mental Health Counseling Today. Get Free No-obligation Guidance by Behaviroal Health Specialists Who Understand Mental Health Recovery.
Similarities Between ASD and PTSD
Symptoms of ASD and PTSD are similar and usually involve a combination of intrusion symptoms (eg, reexperiencing the event), avoidance symptoms, negative effects on cognition and mood (eg, emotional numbing), altered arousal and reactivity, and dissociative symptoms. Both acute stress disorder and PTSD result from experiencing or being exposed to trauma. As a result of the trauma, the individual struggles with a sense of emotional dysregulation, heightened arousal, and a tendency to avoid triggering situations, people, or events.
Acute Stress Disorder Vs PTSD
The most significant difference between ASD and PTSD is the onset and duration of symptoms. The effects of ASD present immediately and last up to a month, while PTSD symptoms present slower and last longer, up to several years if not treated.
Acute stress disorder (ASD) patients are twenty-four times more likely to die from suicide and have twice the risk of all-cause mortality compared to the general population. ASD can lead to chronic PTSD, which is a debilitating psychiatric disorder. PTSD can significantly affect a patient’s quality of life. Due to these risks, managing a traumatic event requires interprofessional care coordination involving providers in various disciplines (such as emergency medicine, psychiatry, orthopedics, and neurosurgery), psychologists, nurses, pharmacists, and social workers. Each area will contribute to the overall care plan based on their expertise and engage in open information-sharing regarding the patient’s case.
Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.
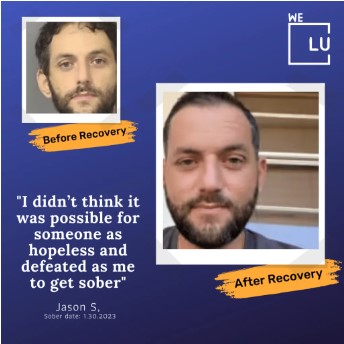


Start a New Life
Begin with a free call to a behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- Comfortable Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
Acute Stress Disorder Vs PTSD Treatment
The following general measures and guidance for ASD and PTSD treatment options are from NCBI: [7]
General Measures:
- Patient Safety – Making sure that the patient is safe after the traumatic event and knows where to seek help in case of an emergency (food and shelter).
- Emotional Support – Patients can receive emotional comfort from close friends or family. Without those, healthcare providers can provide support by explaining the prognosis, course, and coping skills for ASD.
- Practical Support – The process after a traumatic process can be overwhelming. This is because the patient will probably need to help with the police report of the incident, finding a provider, work leave of absence, and health insurance. In case of disability due to an accident, the patient might also need further multi-modal medical support.
- Followups – Regular visits (for six months) for all patients with a significant traumatic event are recommended.
- Suicidality – It is vital to evaluate patients for suicidality in each visit, especially in patients with risk factors for suicide or with comorbid psychiatric diseases (such as depression).
Psychotherapy & Medications for ASD & PTSD:
Psychotherapy – The treatment of choice for acute stress disorder (ASD) is a unique form of cognitive-behavioral therapy (CBT) called trauma-focused CBT. CBT can reduce the risk of further developing PTSD. This evidence-based practice can be delivered via the internet, in person, or by phone. It focuses on increasing knowledge of trauma psychology, symptom management skills, identifying and disputing cognitive distortions, and exposure therapy.
Exposure therapy is a CBT method that involves controlled patient exposure to the traumatic source to relieve the trauma memory, mimicking fear extinction. Exposure therapy is the standard of care for ASD (and PTSD). A transient worsening of the symptoms can appear, but it is not more common than other intervention methods.
Debriefing involves asking the patient to explain the trauma and their feeling about it in the first 72 hours, which is widely available. Studies have not shown the efficacy of debriefing in preventing the development of PTSD, and debriefing is discouraged from routine administration to ASD patients. Crisis intervention encourages patients to avoid maladaptive coping behaviors (such as drinking alcohol).
Pharmacotherapy – Currently, there is no high-quality evidence for a pharmacotherapeutic agent to treat ASD. Serotonin reuptake inhibitors (SRIs) and propranolol were trialed to prevent or treat ASD but showed little efficacy. Evidence for ASD pharmacotherapy is minimal, and most of the recommendations come from research on PTSD.

PTSD pharmacotherapy has been more effective in reducing mood symptoms compared to recurrent memories and avoidance:
- Serotonin Reuptake Inhibitors (SRIs) – SRIs include Selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs). SRIs are the most studied medications for the treatment of PTSD, with favorable results.
- Three SSRIs (fluoxetine, sertraline, and paroxetine) and one SNRI (venlafaxine) have the strongest evidence and are first-line pharmacotherapies for treating PTSD.
- Second-Generation Antipsychotics (SGAs) – Can be used either as monotherapy or augmentation with SRIs. Second-generation antipsychotics are not first-line and are considered in patients with limited response to SRIs and CBT, especially in the presence of associated anxiety and depression. Pharmacotherapy should be started with small doses and gradually increased. In the absence of a clinical benefit, it should be gradually discontinued.
- Benzodiazepines – Benzodiazepines are not generally recommended for the treatment of PTSD. Benzodiazepines are ineffective in the prevention or treatment of PTSD. Benzodiazepine prescription is associated with significant adverse effects and worse outcomes and should be relatively contraindicated in PTSD patients.
- Beta-Blockers – Studies show that propranolol therapy after an acute stressor did not change PTSD incidence but reduced sympathetic symptoms (such as tachycardia and sweating). Current evidence is not strong enough to recommend its routine prescription for PTSD patients.
Other Treatments – There is evidence that ECT (Electroconvulsive therapy) is beneficial for PTSD patients with concurrent depression with the ability to reduce symptoms for both conditions. It is suggested that one known side effect of ECT (i.e., memory disruption) could be used to help patients with severe PTSD. Clinical trials on mood stabilizers (such as topiramate and tiagabine) are limited in number and quality. Treatment arms were no better than the placebo or had a limited effect size. There are reports that lamotrigine or gabapentin were effective treatments for PTSD patients’ nightmares and flashbacks, but more evidence is required to support these medications.
The diagnosis of what is now accepted as Post Traumatic Stress Disorder (PTSD) has changed over the years as we have gained a better understanding of the stress response and its longer-term impact on the body and the brain. PTSD treatment works. Those who have gone through trauma can learn to feel safe in the world and cope with stress.
Deciding to get help and taking steps to start can be hard. There are several effective Acute Stress Disorder vs PTSD treatments. This means you have options. Many professionals provide evidence-based talk therapy and medication to people who go through trauma. Treatments with the strongest evidence should be the first line of treatment for PTSD and ASD whenever possible, considering patient preferences, values, and clinician expertise.
We Level Up FL provides world-class care with round-the-clock medical professionals available to help you cope. All work as a team, providing trauma treatment programs and PTSD Treatment for successful recovery. Make this your opportunity to reclaim your life. Call today to speak with one of our treatment specialists. Your call is private and confidential, and there is never any obligation.
Search Acute Stress Disorder Vs PTSD & Other Resources
Sources:
[1, 4] Acute Stress Disorder Vs PTSD – Veterans Affairs – https://www.ptsd.va.gov/understand/related/acute_stress.asp#:~:text=Acute%20Stress%20Disorder%20(ASD)%20is,about%20ASD%20and%20treatment%20options.
[2,7] Fanai M, Khan MAB. Acute Stress Disorder. [Updated 2022 Jul 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560815/
[3] The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, is the 2013 update to the Diagnostic and Statistical Manual of Mental Disorders, the taxonomic and diagnostic tool published by the American Psychiatric Association.
[5] Post-Traumatic Stress Disorder – https://medlineplus.gov/posttraumaticstressdisorder.html – U.S. Department of Health and Human Services National Institutes of Health
[6] PTSD: National Center for PTSD – Acute Stress Disorder Vs PTSD – Veterans Affairs – https://www.ptsd.va.gov/professional/treat/essentials/acute_stress_disorder.asp#one