Is Depression Genetic?
Depression, like many mental health conditions, is a complex disorder with various contributing factors. While it is not solely caused by genetics, there is evidence to suggest that genetic factors play a significant role in its development. Individuals with a family history of depression are likelier to experience the condition, indicating a genetic predisposition.
A person’s likelihood of experiencing depression is about five times higher if they have a depressed relative than if they don’t. Moreover, anyone who experienced depression as a child may be more prone to developing it themselves. Still, according to studies, the interaction between genes and additional factors (including environment and trauma) determines whether someone experiences depression.
Under certain circumstances, a child who observes a depressive parent or sibling may pick up on that person’s behavior. For instance, children may not find it strange if they keep seeing their parents spending days in bed. Gender might also play a role. According to one study, men only had a 29 percent probability of having inherited depression, whereas women had a 42 percent likelihood.
Genetics is just one piece of the puzzle, and depression’s etiology involves genetic, environmental, and psychosocial factors.
Warning Signs of Genetic Depression
While these signs might indicate a genetic predisposition, depression is a complex condition influenced by multiple factors. Here are the signs and symptoms of genetic depression:
- Family History: Having a close family member, such as a parent or sibling, who has experienced depression.
- Recurrent Episodes: Experiencing multiple episodes of depression or having a chronic, long-term pattern of low mood.
- Early Onset: Developing depression at a relatively young age, especially during adolescence or early adulthood.
- Treatment Resistance: Difficulty responding to standard depression treatments, such as therapy or medication.
- Co-occurring Conditions: Other mental health conditions in the family, such as anxiety disorders or bipolar disorder.
- The severity of Symptoms: Experiencing more severe and persistent symptoms of depression compared to others without a family history.
Risk Factors for Depression
Recognizing these factors can help individuals and their loved ones take proactive steps to promote mental well-being and seek support if needed. If you or someone you care about is experiencing depressive symptoms, seeking professional help is crucial for proper evaluation and appropriate intervention.
Risk factors for depression include the following:
- Family History: Having a family history of depression or other mood disorders.
- Personal History: Having experienced previous depression or other mental health issues.
- Traumatic Life Events: Significant life stressors, such as losing a loved one, relationship problems, or financial difficulties.
- Chronic Illness: Suffering from chronic medical conditions or disabilities.
- Substance Abuse: Using drugs or alcohol excessively can exacerbate or trigger depressive symptoms.
- Social Isolation: Feeling disconnected from others and lacking social support.
- Childhood Adversity: Experiencing abuse, neglect, or adverse experiences during childhood.
- Gender: Women tend to have a higher risk of depression than men.
- Personality Traits: Certain personality traits, like perfectionism or low self-esteem, may increase vulnerability to depression.
- Lack of Coping Skills: Difficulty coping with stress and managing emotions effectively.
Types of Depressive Disorders
There are several types of depression, including major depressive disorder (MDD), characterized by persistent and severe low mood and loss of interest in daily activities, and persistent depressive disorder (PDD), which involves chronic but less severe depressive symptoms lasting two years or more.
Other types include seasonal affective disorder (SAD), postpartum depression (PPD), and bipolar disorder, which includes depressive episodes alternating with manic or hypomanic episodes.
Clinical Depression: A mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life.
Persistent Depressive Disorder: A mild but long-term form of depression.
Bipolar Disorder: Associated with mood swings ranging from depressive lows to manic highs.
Bipolar II Disorder: A type of bipolar disorder characterized by depressive and hypomanic episodes.
Postpartum depression: Depression that occurs after giving birth.
Depression Treatment
Depression treatment typically involves a combination of psychotherapy (such as cognitive-behavioral therapy or interpersonal therapy) and medication (such as antidepressants) to address the symptoms and underlying causes of depression. Moreover, lifestyle changes, support from loved ones, and self-care practices may significantly affect the overall treatment plan.
- Support Group: A place where those pursuing the same disease or objective, such as weight loss or depression, can receive counseling and exchange experiences.
- Cognitive Behavioral Therapy: A conversation treatment that aims to change the negative attitudes, actions, and feelings connected to psychiatric discomfort.
- Counseling Psychology: A subfield of psychology that handles issues with the self that are connected to work, school, family, and social life.
- Anger Management: To reduce destructive emotional outbursts, practice mindfulness, coping skills, and trigger avoidance.
- Psychoeducation: Mental health education that also helps individuals feel supported, validated, and empowered.
- Family Therapy: Psychological counseling that improves family communication and conflict resolution.
The Genetics of Depression Explained
Research has identified specific genes and genetic variations associated with an increased risk of depression. These genes regulate neurotransmitters, brain structure, and the stress response system, critical components of mood regulation.
However, environmental and lifestyle factors also interact with genetic predispositions to influence depression’s onset and severity.
Depression can arise due to a combination of various factors. The exact cause may vary from person to person, but some common triggers include the following:
- Biological Factors: Imbalances in brain chemistry, specifically neurotransmitters like serotonin and norepinephrine, may contribute to depression.
- Genetics: A family history of depression can increase the risk of developing the condition, indicating a genetic predisposition.
- Environmental Stressors: Significant life events such as losing a loved one, trauma, relationship issues, work-related stress, or financial hardships can trigger or exacerbate depressive episodes.
- Psychological Factors: Certain personality traits, coping mechanisms, and negative thought patterns can influence a person’s vulnerability to depression.
It is crucial to recognize that depression is a complex and multifaceted disorder, and the interplay of these factors can contribute to its onset and progression in different individuals.
Genetic Predisposition To Depression
Genetic depression predisposition, scientifically known as genetic susceptibility, refers to the increased likelihood of developing depression due to specific genetic factors inherited from one’s parents or ancestors. Research suggests that individuals with a first-degree relative (parent or sibling) who has had depression are at a higher risk of developing the condition. However, having a genetic predisposition does not guarantee a person will experience depression.
Serotonin and Depression Genetics Link
Serotonin is a neurotransmitter, a chemical brain messenger, crucial in regulating mood, emotions, and behavior. It is often referred to as the “feel-good” neurotransmitter because it contributes to feelings of well-being and happiness.
Genetic studies have identified genes involved in synthesizing, reuptake, and serotonin receptors. Variations in these genes can influence serotonin levels and their functioning in the brain. Some of the most extensively studied genes include the (SLC6A4) serotonin transporter gene and the serotonin receptor genes (e.g., HTR1A, HTR2A).
Individuals with certain genetic variations in these serotonin-related genes may have differences in how their brain processes and responds to serotonin. These genetic variants have been linked with an increased risk of developing depression. For instance, the serotonin transporter gene variant known as the “short” allele has been linked to higher susceptibility to depression in some studies.

Skip To:
Learn More:
- 5 Stages of Depression, Symptoms, Causes, and Effective Treatments
- Crippling Depression Definition, Symptoms & Treatment
- Atypical Depression. What Is It? Symptoms & Treatment
- Situational Depression Symptoms, Causes & Treatment
- Postpartum Depression Treatment, Causes, Symptoms, Anxiety in Pregnancy, & Risks
- What Does Depression Feel Like? Symptoms & Early Signs
- Manic Depression Vs Bipolar. Are They The Same?
- Unipolar Depression Definition, Symptoms & Treatment
- Signs of Depression in Women, Symptoms & Treatment
- How Long Does Postpartum Depression Last?

Is Genetic Depression Curable?
Genetic depression, like all forms of depression, is considered treatable but not necessarily curable in the traditional sense. Genetic factors can influence a person’s susceptibility to depression but do not determine the outcome definitively.
Treatment for genetic depression typically involves a combination of psychotherapy, medication, and lifestyle changes to manage symptoms and improve quality of life. With the right interventions and support, many individuals with genetic depression can experience significant relief from symptoms, achieve remission, and lead fulfilling lives.
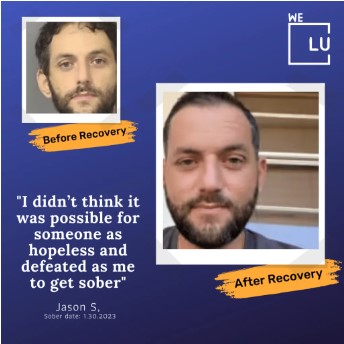
Contact We Level Up mental health treatment center now to get started. We can help you explore treatment options and resources.
World-class, Accredited, 5-Star Reviewed, Effective Mental Health Dual Diagnosis Programs. Complete Integrated Inpatient Rehab with Free Post Discharge Therapy Planning.
CALL (855) 940-6125End the Emotional Pain Rollercoaster. Gain Stability & Happiness Through Recovery Treatment. Start Mental Health Counseling Today. Get Free No-obligation Guidance by Behaviroal Health Specialists Who Understand Mental Health Recovery.
Is Depression Genetic or Environmental? Facts
Genetic Test for Depression
Genetic testing for depression, also known as pharmacogenetic or genetic testing for antidepressants, is a type of DNA analysis that assesses an individual’s genetic makeup to determine how their genes may influence their response to antidepressant medications.
The test examines specific genes related to drug metabolism, neurotransmitter receptors, and other factors involved in medication effectiveness. The information obtained from the genetic test can help healthcare providers make more personalized and informed decisions about antidepressant medication, dosage adjustments, and potential drug interactions, ultimately improving treatment outcomes for individuals with depression.
However, genetics depression testing is just one tool in the overall treatment approach, and treatment decisions should be made in conjunction with a qualified healthcare professional’s guidance.
Types of Genetic Test Depression
There are different types of genetic tests related to depression. Here are three common types:
- Pharmacogenetic Testing: This genetic test analyzes specific genes involved in drug metabolism and neurotransmitter receptors to determine an individual’s response to antidepressant medications.
- Gene Expression Profiling: This test measures the activity levels of specific genes in a person’s blood or brain tissue to assess their genetic predisposition to depression.
- Genome-Wide Association Studies (GWAS): GWAS involves scanning thousands of genetic variations across the entire genome of many individuals with and without depression to identify genetic markers associated with the disorder.
It’s essential to consult with a qualified healthcare professional before undergoing any genetic test for depression to understand the results’ implications and limitations and determine the most appropriate treatment plan based on the individual’s unique needs.
Depression and Genetics
Genetics and depression have a scientific connection. A family history of depression can increase an individual’s risk of developing the condition. However, it is essential to understand that genetics is just one factor contributing to depression, and having a family history does not guarantee that someone will experience depression.
Is depression and anxiety genetic? Stressful life events, trauma, chronic stress, and other environmental factors can play a significant role in developing depression and anxiety.
Moreover, not everyone with a family history of depression will experience the condition, and conversely, some individuals with no family history can still develop depression.


End the Emotional Pain. Get Your Life Back.
Feeling Depressed, Anxious or Struggling with Mental Health Illness? Get Safe Comfortable Mental Health Dual Diagnosis High-Quality Therapy From Counselors That Care. Begin Your Recovery Now.
Hotline (855) 940-6125Genetic Depression Statistics
Heritability studies suggest that genetics accounts for around 30-40% of the risk of developing depression.
One of the most prevalent mental diseases in the US is depression. Some people with severe depression may experience substantial impairments that impede their capacity to engage in meaningful life activities.
21.0 Million
An estimated 21.0 million adults in the US had at least one major depressive episode. This number represented 8.4% of all US adults.
Source: NIMH
10.5%
The prevalence of major depressive episodes was higher among adult females (10.5%) than males (6.2%).
Source: NIMH
25
The prevalence of adults with a major depressive episode was highest among individuals aged 18-25 (17.0%).
Source: NIMH
Is Bipolar Depression Genetic?
Bipolar depression is believed to have a significant genetic component. Research has shown that individuals with a family history of bipolar disorder are at a higher risk of developing the condition. Genetic studies have identified specific genes that may contribute to the susceptibility to bipolar depression, although environmental factors also play a role in its development.
While genetics can increase the likelihood of bipolar depression, a complex interplay between genetic predisposition and environmental influences ultimately contributes to its manifestation.
Is Anxiety and Depression Genetic?
Both anxiety and depression have a genetic component. Research suggests that individuals with a family history of these disorders are likelier to experience them. Genetic studies have identified specific genes and genetic variations associated with an increased risk of developing anxiety and depression. However, genetics is just one factor, and environmental influences, life experiences, and individual coping mechanisms also play significant roles in developing anxiety and depression. The interaction between genetics and environment is complex and can vary from person to person.
Is Postpartum Depression Genetic?
While the exact cause is not fully understood, scientific research suggests a multifactorial etiology involving genetic, hormonal, neurobiological, and psychosocial factors. Genetic studies indicate a heritable component, with certain genetic variations potentially influencing hormonal regulation and neurotransmitter pathways, contributing to the vulnerability of PPD in susceptible individuals.
Postpartum depression (PPD) may have a genetic basis, as research indicates that women with a family history of depression, including PPD, have an increased risk of developing the condition.
Genetic factors could contribute to the hormonal and neurotransmitter changes that play a role in PPD’s onset. However, PPD is a multifaceted disorder influenced by genetics, hormonal fluctuations, psychosocial stressors, and a woman’s coping mechanisms.
While genetics may predispose some women to PPD, the interplay between these genetic factors and environmental influences remains complex and requires further comprehensive understanding. Effective prevention and management strategies for PPD involve addressing genetic susceptibility and the broader contextual factors surrounding childbirth and early motherhood.

End the Emotional Pain. Get Your Life Back.
Feeling Depressed, Anxious or Struggling with Mental Health Illness? Get Safe Comfortable Mental Health Dual Diagnosis High-Quality Therapy From Counselors That Care. Begin Your Recovery Now.
Hotline (855) 940-6125Tips To Prevent Genetic Depression
Preventing genetic depression involves a combination of lifestyle choices, early intervention, and support. Here are some tips:
- Maintain a Healthy Lifestyle: Adopt a balanced diet, exercise regularly, and ensure adequate sleep. These factors can positively impact your mood and overall well-being.
- Manage Stress: Practice stress-reduction techniques like mindfulness, meditation, or yoga to help mitigate the impact of stressors that could trigger depressive episodes.
- Seek Professional Help: If you have a family history of depression or experience symptoms, consult a mental health professional. Early intervention and therapy can help manage and prevent the onset of depression.
- Stay Connected: Cultivate social solid connections and maintain supportive relationships. Social support can act as a buffer against depression and provide emotional resilience.
- Develop Coping Skills: Learn healthy coping mechanisms for life challenges. Effective problem-solving and stress management skills can reduce the risk of depressive episodes.
- Monitor Your Mood: Be mindful of changes in your mood and mental state. Regular self-assessment and awareness can help you identify and address early signs of depression.
- Medication and Therapy: If needed, consult a psychiatrist or healthcare provider. They can recommend appropriate medications and therapies tailored to your needs.
- Genetic Counseling: If you have a known family history of depression, consider genetic counseling to understand better your genetic risk factors and potential strategies for prevention.
- Healthy Habits During Pregnancy: If you plan to have children, maintaining a healthy lifestyle during pregnancy can contribute to both your well-being and your child’s, potentially reducing the risk of postpartum depression.
- Education and Awareness: Educate yourself about depression and its genetic component. Understanding your risk factors empowers you to take proactive steps for prevention.
Depression is genetic. However, while genetics play a role, lifestyle choices and environmental factors can significantly influence the manifestation of genetic predispositions. Individual responses can vary, so it’s essential to tailor prevention strategies to your unique situation with healthcare professionals’ guidance.
Finding Treatment For Depression
Rehabilitation for depression is a comprehensive treatment approach to address the disorder’s physical, emotional, and psychological aspects.
It typically involves a combination of therapies, counseling, medication management, and lifestyle interventions. In rehab, individuals with depression receive specialized care from mental health professionals, such as psychiatrists, therapists, and social workers, who collaboratively develop a personalized treatment plan.
The goal of rehab for depression is to help individuals regain control over their lives, learn coping strategies, and acquire the necessary skills to manage their symptoms and prevent relapses.

First-class Facilities & Amenities
World-class High-Quality Mental Health Services & Behavioral Health Substance Abuse Treatment
Rehab Centers TourRenowned Mental Health Centers. Serene Private Facilities. Inpatient Rehab Programs Vary.
Mental Health Helpline (855) 940-6125Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Successes
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Development Events
- Comfortable Onsite Medical Detox Center
Top 4 Can Depression Be Genetic? FAQs
-
Is depression hereditary or genetic?
Depression is both hereditary and genetic. This means that while a family history of depression can increase the risk of developing the condition, genetic variations inherited from parents can also contribute to an individual’s susceptibility to depression.
-
How is depression genetic?
Depression is considered genetic because specific genes and genetic variations can influence neurotransmitter function, brain structure, and stress response systems, all affecting mood regulation. These genetic factors inherited from parents can contribute to an individual’s predisposition to developing depression, but environmental and lifestyle factors also interact with genetics to influence its onset and severity.
-
Is there genetic testing for depression medications?
Depression genetic testing for medications is available and gaining popularity. Pharmacogenetic testing analyzes a person’s genetic profile to identify how their genes may affect their response to specific antidepressant medications. This information can help healthcare providers make more informed decisions about which medications may be more effective and better tolerated for individual patients, potentially improving treatment outcomes and reducing the risk of adverse reactions. However, it is essential to consult a qualified healthcare professional to determine the appropriateness and benefits of genetic testing for depression medications in each case.
-
How does genetic testing depression work?
Genetic testing for depression involves analyzing a person’s DNA to identify genetic variations that may influence their response to antidepressant medications. The test examines genes related to drug metabolism, neurotransmitter receptors, and other factors involved in medication effectiveness, providing information to healthcare providers about potential drug interactions, dosage adjustments, and medication selection tailored to the individual’s genetic makeup.
Clinical Depression Video. Depression Symptoms. Signs of Depression. Major Depressive Disorder Help.
Is depression genetics? Are you genetically depressed? To be diagnosed with depression, a person must experience a persistent low mood or loss of interest in most activities, lasting at least two weeks. Moreover, they may exhibit other symptoms, such as the following:
- Changes in appetite.
- Sleep disturbances.
- Fatigue.
- Feelings of worthlessness or guilt.
- Difficulty concentrating.
- Thoughts of self-harm or suicide.
A professional mental health evaluation is essential to accurately diagnose depression and determine the appropriate treatment, including therapy, medication, or a combination.
If you or a loved one is struggling with depression, anxiety, or other mental health disorder(s), call for a FREE consultation 24/7 at (561) 678-0917
Get FREE mental health treatment insurance check – https://welevelup.com/rehab-insurance/
Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.


Start a New Life
Begin with a free call to a behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- Comfortable Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
Search We Level Up FL Is Depression Genetic? Mental Health Topics & Resources
Sources
[1] Is Depression Genetic? Related Topic. National Institute of Mental Health – ‘Depression’ (www.nimh.nih.gov)
[2] Is Depression Genetic? Related Topic. U.S. Food and Drug Administration (FDA) (www.fda.gov/)
[3] Depression Treatment » We Level Up Treatment Center Is Depression Genetic? Related Topic.
[4] Shadrina M, Bondarenko EA, Slominsky PA. Genetics Factors in Major Depression Disease. Front Psychiatry. 2018 Jul 23;9:334. Doi 10.3389/fpsyt.2018.00334. PMID: 30083112; PMCID: PMC6065213. Is Depression Genetic? Related Topic.
[5] Alshaya DS. Genetic and epigenetic factors associated with depression: An updated overview. Saudi J Biol Sci. 2022 Aug;29(8):103311. Doi 10.1016/j.sjbs.2022.103311. Epub 2022 May 20. PMID: 35762011; PMCID: PMC9232544. Is Depression Genetic? Related Topic.
[6] Associations Between Depression in Parents and Parenting, Child Health, and Child Psychological Functioning. Available from: https://www.ncbi.nlm.nih.gov/books/NBK215128/ Is Depression Genetic? Related Topic.
[7] Behere AP, Basnet P, Campbell P. Effects of Family Structure on Children’s Mental Health: A Preliminary Study. Indian J Psychol Med. 2017 Jul-Aug;39(4):457-463. Doi 10.4103/0253-7176.211767. PMID: 28852240; PMCID: PMC5559994. Is Depression Genetic? Related Topic.
[8] Postpartum depression – Office on Women’s Health (.gov) Is Depression Genetic? Related Topic.
[9] The most extensive genome study of depression to date reveals genetic risk factors – Veterans Affairs (.gov) Is Depression Genetic? Related Topic.
[10] Study of Genetic Differences in People With Depression – Clinical Trials (.gov) Is Depression Genetic? Related Topic.






