What is Persistent Depressive Disorder?
Persistent depressive disorder (PDD, also known as dysthymia) is a constant and long-term form of depression. It involves feeling sad, losing interest in daily activities, and struggling to accomplish tasks. You feel sad or down for most of the day, nearly every day, lasting two years or more.
While not as severe as major depression, your current depressed mood can range from mild to severe.
Because persistent depressive disorder lasts a long time, dealing with its symptoms can be challenging. Combining talk therapy and medication can be a helpful way to treat this condition.
What are Persistent Depressive Disorder Symptoms?
Persistent depressive disorder may feel like a constant weight of sadness and a lingering sense of low energy, making daily activities challenging. The main symptom is having a down or dark mood.
Dysthymia symptoms can significantly disrupt your life and may include:
- Feeling sad, empty, or down.
- Losing interest in daily activities.
- Fatigue and lack of energy.
- Low self-esteem, self-criticism, or feeling incapable.
- Difficulty focusing and making decisions.
- Challenges in completing tasks effectively and on time.
- Quick irritability, impatience, or anger.
- Avoidance of social activities.
- Feelings of guilt and dwelling on the past.
- Changes in appetite or overeating.
- Sleep disturbances.
- The overall sense of hopelessness.
Many individuals with PDD also experience an episode of major depression at least once, a phenomenon sometimes referred to as “double depression.”
What Causes Persistent Depressive Disorder?
The causes of persistent depressive disorder (dysthymia) include a combination of genetics, biological, environmental, and psychological factors.
- Genetic Factors: A family history of depression may increase the likelihood of developing persistent depressive disorder.
- Biological Factors: Imbalances in brain chemicals, neurotransmitters, or hormonal changes may play a role in the onset of persistent depressive disorder.
- Environmental Influences: Stressful life events, trauma, or chronic stress can contribute to the development and persistence of depressive symptoms.
- Psychological Factors: Personality traits, coping mechanisms, and thought patterns may influence susceptibility to persistent depressive disorder.
- Neurological Factors: Abnormalities in brain structure or function may be associated with the development of this disorder.
- Early Childhood Experiences: Adverse experiences during childhood, such as abuse or neglect, may increase the risk of persistent depressive disorder later in life.
How Common is Persistent Depressive Disorder?
Persistent depressive disorder (PDD) can affect individuals of any age, with over 3% of the U.S. population experiencing it at some stage in their lives. It is more prevalent in women and tends to occur more frequently in individuals with family members who also have the condition.
How is Persistent Depressive Disorder Diagnosed?
PDD or dysthymia is typically diagnosed through a comprehensive assessment by a mental health professional. This evaluation involves discussing the individual’s symptoms, medical history, and family history of mental health issues.
The diagnostic criteria outlined in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders), which includes the presence of a sad or low mood for most of the day, nearly every day, over at least two years, is often used to confirm the diagnosis.
Also, the clinician may rule out other potential causes for the symptoms through medical and psychological evaluations.
How is Persistent Depressive Disorder Treated?
Persistent depressive disorder is often treated with a combination of psychotherapy, medication, and lifestyle changes. Talking therapies like cognitive-behavioral therapy (CBT) can help address negative thoughts and improve relationships. Medications, such as antidepressants, may be used to regulate brain chemicals and ease symptoms.
Alongside these treatments, making lifestyle adjustments like regular exercise, good sleep habits, and stress management can also help manage depression. Individuals must collaborate with their healthcare providers to find a tailored treatment plan, regularly checking progress and adjusting the approach.
Persistent Depressive Disorder Medication
Persistent Depressive Disorder Medication
Medications commonly prescribed for persistent depressive disorder include antidepressants, which aim to regulate neurotransmitters in the brain.
Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are often preferred.
These medications work by increasing the levels of certain neurotransmitters, helping to alleviate persistent depressive symptoms.
Individuals must work closely with their healthcare providers to determine the most suitable medication and dosage based on their needs and potential side effects. Regular monitoring and open communication about any changes or concerns during medication use are essential aspects of managing persistent depressive disorder with medication.
Persistent Depressive Disorder Therapy
Persistent Depressive Disorder Therapy
Therapeutic approaches for persistent depressive disorder include:
- Cognitive-Behavioral Therapy (CBT): Focuses on identifying and changing negative thought patterns and promoting healthier behaviors and coping strategies.
- Interpersonal Therapy (IPT): Addresses interpersonal issues and relationships, helping individuals improve communication and navigate social challenges.
- Psychodynamic Therapy: Explores unconscious thoughts and emotions to understand and resolve internal conflicts contributing to depressive symptoms.
- Mindfulness-Based Therapies: Incorporates mindfulness and meditation techniques to enhance awareness, reduce stress, and promote emotional well-being.
- Behavioral Activation: Targets patterns of avoidance and withdrawal, encouraging individuals to engage in positive and rewarding activities.
- Dialectical Behavior Therapy (DBT): Combines cognitive-behavioral techniques with mindfulness, emphasizing emotional regulation and interpersonal skills.
Individuals may work with their therapists to determine the most effective therapeutic approach based on their unique needs and preferences.
Skip To:
Learn More:
- What is Mild Depression? Symptoms and Treatment
- What is Crippling Depression? Learning How To Deal With Crippling Depression
- Atypical Depression. What Is It? Symptoms and Treatment
- Learn How to Cope with Depression. 10 Ways to Cope with Depression.
- Manic Depression Vs Bipolar. Are They The Same?
- Situational Depression Vs Clinical Depression, Symptoms, Causes, and Treatment
- Unipolar Depression Definition, Causes, Symptoms, and Treatment
- What Does Depression Feel Like? Symptoms and Early Signs
- Signs Of Depression In Women, Symptoms and Treatment
- Effective Depression Treatment, Depressive Disorder Symptoms, Types, and Causes
Am I Depressed? Free Quiz
Many people experience persistent depression, and it can affect how you handle everyday things, such as work and relationships. Are you worried if you’re experiencing depression now? Take the quiz below to explore if you may be experiencing symptoms associated with depression.
This quiz is not a substitute for professional diagnosis, so seek guidance from a mental health professional for an accurate assessment.
Get persistent depressive disorder counseling that works. Discover professional help from We Level Up Florida’s mental health therapists. Start getting support with a free call to our mental health hotline.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Dual Diagnosis Mental Health Centers Near You?
Even if therapy failed previously, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about counseling alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
FREE 24/7 Dual Diagnosis Mental Health Services Hotline
Persistent Depressive Disorder Self-Care Strategies
Self-care is crucial for managing persistent depressive disorder. Here are some strategies:
- Establish a Routine: Create a daily schedule to provide structure and stability.
- Regular Exercise: Engage in physical activity, positively impacting mood and overall well-being.
- Healthy Sleep Habits: Prioritize good sleep hygiene to improve sleep quality.
- Nutritious Diet: Maintain a balanced diet with nourishing foods to support physical and mental health.
- Mindfulness and Relaxation Techniques: Practice mindfulness, deep breathing, or meditation to reduce stress.
- Social Connections: Foster positive relationships and seek support from friends and family.
- Limit Stressors: Identify and manage sources of stress, setting realistic goals and boundaries.
- Hobbies and Enjoyable Activities: Engage in activities that bring joy and a sense of accomplishment.
- Limit Substance Use: Avoid excessive alcohol or substance use, as they can worsen depressive symptoms.
- Therapeutic Journaling: Write down thoughts and feelings to gain insight and release emotions.
Individuals should tailor these strategies to their preferences and consistently incorporate them into their daily lives for effective self-care.
We Level Up FL Persistent Depressive Disorder Treatment Tips
✅ Attend therapy sessions regularly and communicate openly with your healthcare provider about your experiences and concerns.
✅ Take prescribed medications as directed, and don’t hesitate to discuss any side effects or adjustments needed.
✅ Prioritize self-care by maintaining a routine, engaging in physical activity, fostering positive relationships, and practicing stress-reducing techniques like mindfulness or deep breathing.

End the Emotional Pain. Get Your Life Back.
Feeling Depressed, Anxious or Struggling with Mental Health Illness? Get Safe Comfortable Mental Health Dual Diagnosis High-Quality Therapy From Counselors That Care. Begin Your Recovery Now.
Hotline (855) 940-6125What’s the Difference Between Major Depressive Disorder Vs Persistent Depressive Disorder?
Major depressive disorder (MDD) and persistent depressive disorder (PDD) are two types of depression with differences in how long symptoms last and their intensity. MDD involves:
- Severe episodes lasting at least two weeks.
- It features intense symptoms like weight changes.
- Sleep disruptions.
- Thoughts of suicide.
MDD can recur with periods of improvement, impacting various aspects of daily life. In contrast, persistent depressive disorder (PDD), also called dysthymia, lasts for two years or more with generally milder but enduring symptoms.
PDD affects daily life over the long term, even if symptoms don’t meet the criteria for a major depressive episode. The chronic nature of PDD distinguishes it from the episodic pattern of MDD.
First-class Facilities & Amenities
World-class High-Quality Mental Health Services & Behavioral Health Substance Abuse Treatment
Rehab Centers TourRenowned Mental Health Centers. Serene Private Facilities. Inpatient Rehab Programs Vary.
Mental Health Helpline (855) 940-6125Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Successes
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Development Events
- Comfortable Onsite Medical Detox Center
Can I Prevent Persistent Depressive Disorder?
While it may not always be possible to PDD, there are steps you can take to reduce the risk or mitigate its impact:
- Early Intervention: Seek professional help if you notice persistent feelings of sadness or changes in mood. Early intervention can be crucial in managing depressive symptoms.
- Healthy Lifestyle: Adopt a healthy lifestyle that includes regular exercise, a balanced diet, and sufficient sleep. These factors contribute to overall well-being and may help mitigate the risk of depression.
- Stress Management: Develop effective stress management techniques, such as mindfulness, relaxation exercises, or hobbies, to cope with life’s challenges and reduce the impact of stress on mental health.
- Supportive Relationships: Foster positive relationships and maintain a solid support system. Social connections can provide emotional support and resilience against depressive symptoms.
- Regular Check-ins: Stay aware of your mental health and regularly check in with a mental health professional. Discuss any concerns or changes in mood to address potential issues early on.
While these strategies may not guarantee prevention, they can contribute to overall mental well-being and potentially reduce the risk or severity of persistent depressive disorder.
Suppose you or someone you know is dealing with depression, which affects their daily functioning. In that case, We Level Up Florida Mental Health Treatment Center provides personalized care with a team of experienced professionals. Begin your journey towards better health by taking the first step towards healing. Get help. Call We Level Up FL now. Each call is free and confidential.
World-class, Accredited, 5-Star Reviewed, Effective Mental Health Dual Diagnosis Programs. Complete Integrated Inpatient Rehab with Free Post Discharge Therapy Planning.
CALL (855) 940-6125End the Emotional Pain Rollercoaster. Gain Stability & Happiness Through Recovery Treatment. Start Mental Health Counseling Today. Get Free No-obligation Guidance by Behaviroal Health Specialists Who Understand Mental Health Recovery.
Therapist Tips to Cope and Combat Depressive Episodes
Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.
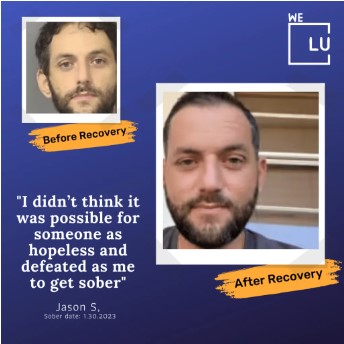


Start a New Life
Begin with a free call to a behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- Comfortable Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
Search We Level Up FL Persistent Depressive Disorder Treatment, Mental Health Topics & Resources
Sources
[1] Dysthymia Vs Depression – PMC – National Center for Biotechnology Information (NCBI)
[2] What is Dysthymia? – StatPearls – National Institutes of Health (NIH)
[3] Dysthymia Disorder – National Institute of Mental Health (NIMH)
[4] Dysthymia Definition – MedlinePlus (.gov)
[5] Chand SP, Arif H. Depression. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430847/
[6] What is Depression? – Substance Abuse and Mental Health Services Administration (SAMHSA)
[7] Depression Medicines – Food and Drug Administration (FDA)
[8] Depression: MedlinePlus Medical Encyclopedia
[10] Depression Treatment For Veterans – Veterans Affairs (.gov)